Steve Jobs was right to be optimistic when, in 2004, he announced that he had cancer in his pancreas. Although cancer of the pancreas has a terrible prognosis—half of all patients with locally advanced pancreatic cancer die within 10 months of the diagnosis; half of those in whom it has metastasized die within six months—cancer in the pancreas is not necessarily a death sentence.
The difference is that pancreatic cancers arise from the pancreatic cells themselves; this is the kind that killed actor Patrick Swayze in 2009. But cancers in the pancreas, called neuroendocrine tumors, arise from islands of hormone-producing cells that happen to be in that organ. Jobs learned in 2003 that he had an extremely rare form of this cancer, an islet-cell neuroendocrine tumor. As the name implies, it arises from islet cells, the specialized factories within the pancreas that produce and secrete insulin, which cells need in order to take in glucose from the food we eat. Unlike pancreatic cancer, with neuroendocrine cancer “if you catch it early, there is a real potential for cure,” says cancer surgeon Joseph Kim of City of Hope, a comprehensive cancer center in Duarte, Calif.
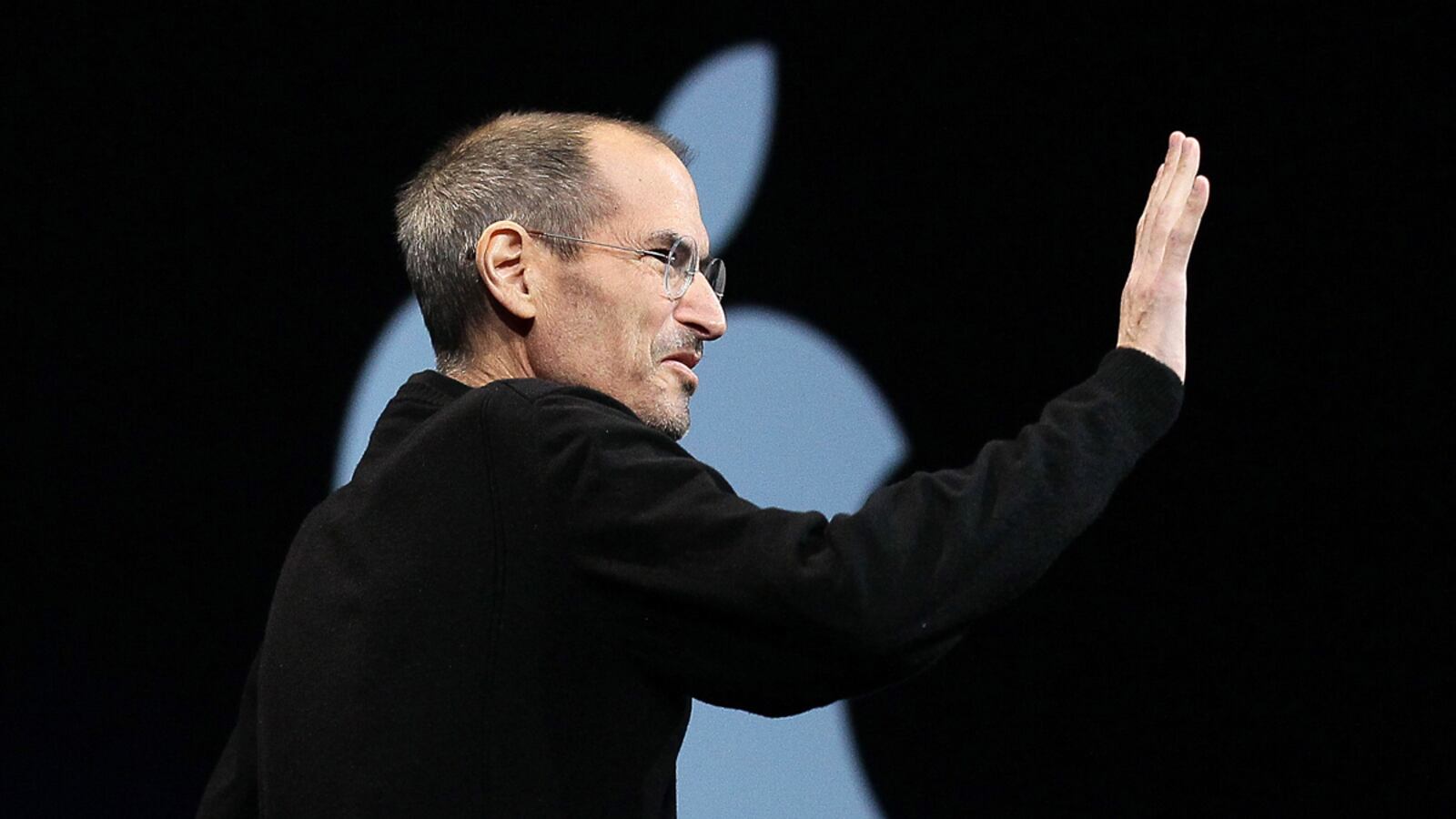
But although neither Apple nor those close to Jobs were willing to discuss the treatments he elected or the course of his disease, interviews with experts on neuroendocrine tumors suggest that some of the choices he made did not extend his life and may have shortened it.
The cancer was detected during an abdominal scan in October 2003, as Fortune magazine reported in a 2008 cover story. It was 7:30 in the morning, Jobs said in his 2005 commencement address at Stanford University. He reportedly had the scan—which is seldom done, much less advised, as a routine part of a physical—because he had a history of gastrointestinal problems, but he also may have been experiencing symptoms, most likely gastrointestinal ones. Those tend to arise from the hormone that the particular neuroendocrine tumor produces, explains medical oncologist Matthew Kulke of Dana-Farber Cancer Institute in Boston. In Jobs’s case, that was insulin. (Other neuroendocrine tumors produce gastrin, glucagon, and other digestive hormones.) The main effect of high insulin levels is a profound drop in blood sugar, says surgeon John Chabot of Columbia University Medical center, which can lead to shakiness, cold sweats, nausea, vomiting, blackouts, and neurological changes such as impaired judgment, moodiness, irritability, apathy, and confusion.

There is virtually no debate about the best treatment. “It has long been held that surgery can lead to very long-term survival,” says Kim. In a 2010 analysis of cancer registries, he and colleagues found that patients with neuroendocrine cancer who were eligible for surgery (the cancer has not spread beyond the pancreas) “can have outstanding outcomes,” living for many more years. In part, that is because neuroendocrine cancers tend to be quite slow growing, or indolent. Even those that have been present for years, and in some cases decades, often stay safely confined to the pancreas. This kind of cancer can be so indolent that patients often die with it than from it. Although an estimated 2,000 to 3,000 people in the U.S. are diagnosed every year with neuroendocrine tumors of the pancreas, autopsies find the disease in hundreds more—people who were apparently not harmed by this very slow-growing cancer.
Despite the expert consensus on the value of surgery, Jobs did not elect it right away. He reportedly spent nine months on “alternative therapies,” including what Fortune called “a special diet.” But when a scan showed that the original tumor had grown, he finally had it removed on July 31, 2004, at Stanford University Medical Clinic. In emails to Apple employees immediately after, Jobs said his form of cancer “can be cured by surgical removal if diagnosed in time (mine was),” and told his colleagues, “I will be recuperating during the month of August, and expect to return to work in September.” Despite the delay in having the surgery, Jobs’s upbeat report was not unrealistic: most patients diagnosed with neuroendocrine tumors in the pancreas live at least another 10 years.
Not that the surgery was a walk in the park. In many cases, says Kim, “you can just remove the tumor with a little of the surrounding [pancreatic] tissue.” But Jobs’s was not such a simple case. He underwent an operation called a modified Whipple procedure, or a pancreatoduodenectomy, Fortune reported. The surgery removes the right side of the pancreas, the gallbladder, and parts of the stomach, bile duct, and small intestine. The fact that so much more than the pancreas itself had to be removed suggests that Jobs’s cancer had spread beyond the pancreas. The cancer might have already spread by the time it was discovered in 2003, though Jobs’s sanguine description of his prognosis suggests that if that were the case, the metastasis might have been so small— “micrometastases”—as to be undetectable. Alternatively, the cancer could have spread during the nine months that Jobs was experimenting with nonstandard therapies.
Within five years, it was clear that Jobs was not cured. He underwent a liver transplant at Methodist University Hospital in Memphis in 2009. That strongly suggests the cancer had spread beyond the digestive system that was the focus of the surgery and into the organ that is one of the most common sites of metastasis. Liver transplants are a well-established treatment for tumors that originate in that organ, such as hepatocellular cancer, says City of Hope’s Kim. But removing the liver because it has become riddled with tumors that originated elsewhere is rare. For one thing, liver metastases probably mean the cancer is elsewhere, too, such as in the bones or brain. Swapping out a cancer-ridden liver for a new one may therefore buy some time, but not much.
It can even be counterproductive. Transplant patients need massive doses of immune-suppressing drugs to keep their bodies from rejecting the foreign organ. Although experts differ on how big a role the immune system plays in keeping cancer, especially micrometastases, in check, there is a consensus that it provides some benefit. “Immune-suppressing drugs after a liver transplant for hepatocellular cancer are therefore a major concern,” says Kim. “They may increase the risk of recurrence.” A more standard treatment is to remove only those parts of the liver that contain malignant cells. “If there are a limited number of such spots, we recommend surgeons go in and take them out,” says Kulke. Since the liver regenerates, “that can be curative—or at least it can let patients do a lot better.” Presumably, Jobs was being carefully monitored by his physicians, so it is odd that the liver would suddenly be so riddled with metastases—especially given that neuroendocrine tumors are usually indolent—that more limited, targeted surgery was rejected in favor of a full, and risky, transplant.
Fewer than two dozen cases of liver transplant after metastatic neuroendocrine cancer have been reported in the medical literature. The first such studies were done in France, with surgeons reporting the first results in 1997. Based on 31 cases, including three patients who had a Whipple procedure similar to Jobs’s, they calculated that 59 percent of patients survived at least one year, 47 percent were alive at three years, and 36 percent survived five years or more. The rates were better for the kind of neuroendocrine cancer Jobs had: 69 percent of patients with metastatic carcinoid tumors were alive at five years. But less extreme surgery arguably offers more hope. In a 2003 study, surgeons at the Mayo Clinic found that when only those parts of the liver that are riddled with neuroendocrine metastases (which Jobs apparently had) are removed, half of patients live 45 months or more. This surgery, they concluded, “adds many months of symptom-free survival to the lives of most patients.” In contrast, with a liver transplant “the overall costs and complications ... override its benefits, especially when compared with partial [removal of the liver].” Indeed, liver transplants for metastatic cancer “have been largely abandoned,” says Columbia’s Chabot, because the immune-suppressing, anti-rejection drugs “lead to such a high recurrence rate. If there are spots of metastasis in the liver, it’s better just to remove them. Often, that can let you stay ahead of the disease for another eight to 10 years.” (The liver is one of the few human organs that regenerates, so having pieces removed usually does not impair function.)
Jobs was relieved that, as he put it in that 2004 email, he did “not require any chemotherapy or radiation treatments.” He took that as a sign that the surgery “got it all,” as every cancer patient desperately wishes to hear. In fact, any surgeons who say they “got it all” should be slapped: no existing technology can detect micrometastases, let alone a few million rogue malignant cells floating in the bloodstream or lymph fluid and just waiting to invade some vital organ. If Jobs did not receive chemotherapy, he might have reduced his chances of survival. One of the few bright spots when it comes to neuroendocrine cancer was the Food and Drug Administration’s decision, in May 2011, to approve two new drugs against the disease. One, called Sutent, from Pfizer, was previously approved for the treatment of kidney cancer; it is an angiogenesis inhibitor, targeting the blood vessels that tumors require for their survival. Specifically, it targets a molecule called VEGF that sends signals that promote the growth of blood vessels. “Neuroendocrine tumors are highly vascularized”—full of blood vessels on which they depend for nutrients, says Kulke. “So angiogenesis inhibitors might be a very good start.” The other newly approved drug, Afinitor from Novartis, is what’s called an mTOR inhibitor. It blocks signals involved in both cell proliferation and angiogenesis. According to research in the New England Journal of Medicine, both drugs roughly double progression-free survival from 5.5 months to 11.
Why do neuroendocrine tumors kill? Not because they destroy the insulin-producing cells. As Kulke points out, “you can take insulin injections. But if the cancer metastasizes, you can get wasting and weakness.” Indeed, some 90 percent of cancer fatalities are the result of the metastasis rather than the primary tumor.