If the stars align, the United States may yet be able to vaccinate its way out of the COVID-19 epidemic. The Biden administration says it has procured adequate amounts of highly effective vaccines so that any adult who wants to get a shot may now do so. By June or July, if we immunize most American adults and adolescents, levels of virus transmission will decrease precipitously. In an epidemiological modeling study with the CUNY School of Public Health, we found that roughly three-quarters of the susceptible U.S. population would need to be vaccinated to significantly slow or stop virus transmission. However, the new B.1.1.7 (United Kingdom) variant, among others now accelerating across the country, is more transmissible than the original virus lineages examined in our study. This means even higher levels of vaccine coverage, possibly 80 percent or higher, may be necessary.
Achieving that high bar of vaccination coverage should cause steep drops in levels of coronavirus community transmission, based on emerging data that our vaccines reduce both symptomatic illness and infection. Ideally, this might mean bring us back to virus containment mode, defined (by some) as under one new case per 100,000 residents per day. While the risk of contracting COVID-19 won’t hit zero in such a scenario, most Americans could safely eat in restaurants, drink in bars, dance in clubs, and attend indoor and outdoor concerts or sporting events. They could probably do so without masks, although some with underlying conditions (or those who won’t accept any level of risk) may choose to continue wearing them. This would also mean we could feel even more comfortable with air travel domestically within the U.S. and possibly Canada, or a few other countries where transmission has also slowed.
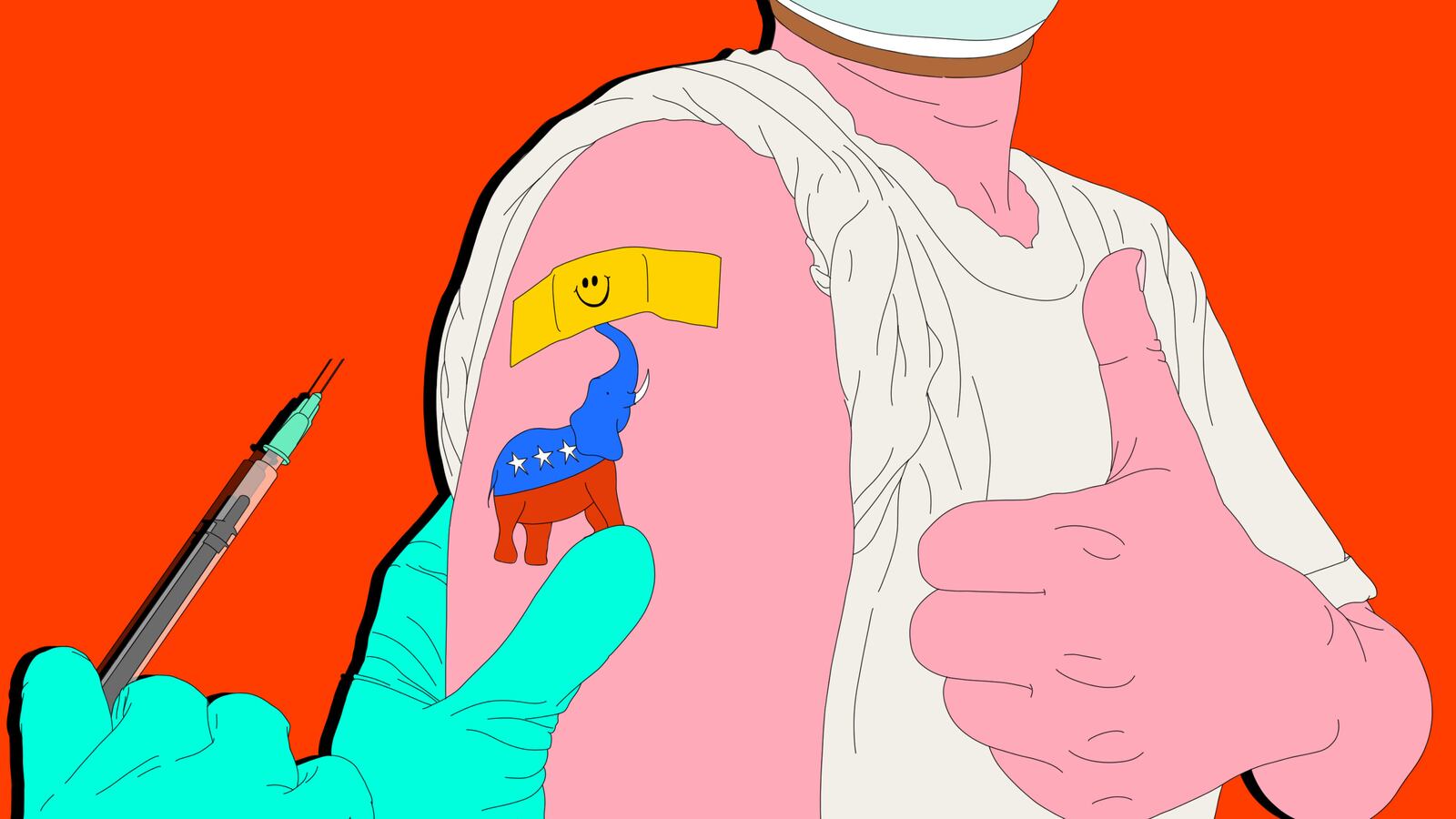
However, surveys and polls consistently point to a problem that could prevent us from achieving our public health goals—no matter what the vaccine technology, distribution, or effectiveness. While vaccine hesitancy cuts across the political spectrum, conservative groups dominate this space, and the U.S. still hasn’t figured out how to reach those holdouts.
An April Monmouth University poll found 43 percent of Republicans said they would not get a COVID-19 vaccine versus just 5 percent of Democrats. Another April Quinnipiac University poll also showed Republicans leading vaccine-hesitant groups, with 45 percent saying they did not plan to get vaccinated against COVID-19. In March, a PBS NewsHour/NPR/Marist poll found similar results, identifying Republicans as the single most vaccine-hesitant group. Vaccine acceptance is particularly low among white, rural southerners, and this is reflected in the fact that states such as Mississippi, Alabama, Louisiana, and Georgia rank at the bottom COVID-19 vaccinations, as do Republican-dominated states like Idaho, Texas, and Wyoming.
If we assume roughly 25 percent of adult Americans identify themselves as Republicans, the poll numbers above would suggest that approximately 10 percent of U.S. adults won’t accept COVID-19 vaccinations in part because they harbor right-wing, anti-vaccine views. Given that some 20 percent of Americans are currently under the age of 15 and therefore are ineligible to receive COVID-19 vaccinations at all, this bloc of vaccine-refusing Republican adults jeopardizes our ability to reach the threshold of herd immunity and could stall a safe reopening.
Exactly how we got to a place where a GOP political affiliation translates to vaccine hesitancy or refusal is complicated. Many of us in the vaccine science community who routinely go up against anti-vaxxer groups have noticed with alarm the increasing politicization around health issues for years. This coincided with the rise of an aggressive “health freedom” movement linked to the Tea Party and the formation of well-organized and funded political action committees (PACs), which sometimes successfully lobbied state legislatures to loosen vaccination requirements for schools, which in turn resulted in many significant pockets of immunization declines, including many counties in Republican-majority red states. Others have noted how anti-vaccine activities were already becoming mainstream in the GOP even prior to COVID-19, and then in 2020, health-freedom defiance expanded to masks and social distancing.
Objections to vaccines, masks, and open expressions of contempt for science are no longer relegated to the extreme or fringe elements of conservatism. And even as many Americans have cheered vaccine numbers ticking up in the last few weeks, we’ve seen the regular expression of COVID-19 anti-vaccine attitudes on Fox News and other conservative news outlets, as well as attacks on me and other scientists.
Now even Republican members of Congress openly espouse anti-vaccine views and refuse COVID-19 immunizations, as Republican-majority state governors and lawmakers prepare executive orders and bills to pre-empt vaccine mandates or so-called passports. The fact that President Donald Trump refused to receive his COVID-19 vaccine in public did not help this situation, nor did his new assertion that Pfizer has a cozy relationship with the FDA and helped to sabotage the J&J vaccine. (However, I was pleased to see Ivanka Trump publicly announce her COVID-19 vaccination.)
We must engage in new outreach to conservative groups, to highlight both the safety and efficacy of COVID-19 vaccines and the urgency for all Americans. This includes debunking misinformation from conservative groups that claim we are already achieving herd immunity, or that young people are not at risk for severe disease and therefore don’t need to be vaccinated, or that those with past COVID-19 infections are already immune. (Worse are the conservative activists, including doctors, who make outrageous claims regarding COVID-19 vaccine safety.)
Ultimately, we must find a way to delink anti-vaccine defiance and political allegiance to the GOP—and as a medical expert, rather than a political scientist, I don’t claim to know all the answers here. But we know that the impact of advocacy and reaching out can be profound. For example, vaccine refusal and hesitancy were also high in Black and Brown communities across the country, but this has declined significantly, according to some polls.
I’ve been going on podcasts, zoom calls, and radio programming that reach Black communities, including some church groups, to learn that the clergy have helped lead efforts in defusing vaccine misinformation and encouraging vaccines. We still have work to do, and now organizations such as the Rockefeller Foundation have prioritized vaccine equity in communities of color. Increasingly, such activities now center more on urgency in ensuring vaccine access rather than combatting hesitancy.
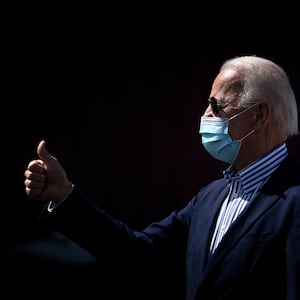
While I go on conservative news outlets whenever invited, this is not nearly enough. I would encourage the Biden administration to do more outreach to key Republican stakeholders and identify ways for reducing vaccine hesitancy, or even host a White House summit on this topic. This process has begun, but much more is required, including enlisting leaders of the GOP, major conservative podcasters and influencers, and governors in Republican-majority states. There may be policy levers to pull and push, including financial incentives for the states. (The administration touted tax credits for employers and other incentives to encourage vaccination as part of its plan to reach more people on Wednesday, but we have to do a lot more.)
As a vaccine scientist in Texas, I would be willing to serve as a “vaccine ambassador” for the Biden administration and meet with leaders in Republican strongholds across the South and Upper Midwest and Mountain states. I’m confident others would as well. Cultivating conservative vaccine champions from the realms of science, politics, and entertainment could expand into a new advocacy push from the federal government.
Reaching holdouts in Democratic constituencies isn’t enough. The government needs a plan to get more of the people actively resistant to the vaccine on the right.
We really have no choice. If we fail to fully vaccinate the American people, virus transmission could continue at a significant level. It would be highest in pockets of low vaccine coverage due to vaccine refusal; a disturbing study from the CDC on Wednesday found that a single unvaccinated healthcare worker in Kentucky sparked an outbreak at a nursing home that killed three people, one of whom was vaccinated. In addition to seeing ongoing hospitalizations, holdout zones could become areas where teachers and essential workers—even vaccinated ones—might feel unsafe. Ultimately, these geographic pockets of accelerated virus transmission might enable the emergence of new virus variants of concern that could escape the protection afforded by our current COVID-19 vaccines. In that case, the entire nation is placed at risk.
In other words, this is urgent. By summer, we must find a way to close the current gap if we are to fully protect the American people. And so far, the administration isn’t coming close.