In 1877, a German pharmacologist named Rudolf Boehm discovered something crazy. By pushing on the chest of a cat, he could keep the animal alive if it wasn’t breathing. In 1891, a German surgeon named Friedrich Maass tried this on people, saving two young patients.
If this trick sounds familiar to you, it’s because these are chest compressions, a critical part of CPR (cardiopulmonary resuscitation). Unfortunately for everyone, Boehm and Maass were early to the party—their discovery didn’t catch on until a half-century later. Major breakthroughs in resuscitation science have been just as slow to follow. In addition to using CPR, today’s doctors can dramatically cool people’s bodies to keep them alive and save individual organs from people being taken off life support for transplantation into patients in need.
But these achievements, while paramount to the evolution of medicine, fall short of a larger goal that a much smaller, much more eccentric group of people have been obsessed with: reversing death itself. Reviving a seemingly dead person or saving a “dead” organ just isn’t the same.
That’s not for a lack of trying. Back in 18th century Amsterdam, people started to realize that, in some cases, the “apparently dead” were not always “actually dead.”
“People keep calling falling into the canals, and they get fished out, and then they get sort of, you know, thumped on until the water comes out, and they… are resuscitated,” Caitjan Gainty, a historian of health and health care at King’s College London, told The Daily Beast.
And thus the idea that death could, in certain circumstances, be reversed, spread across Europe. “Humane societies” began promoting idiosyncratic methods of resuscitation, usually emphasizing stimulating the body, keeping it warm, and generally restarting the “body-machine.” Some methods were simple: rubbing, massaging, and changing the position of the body were common. Other methods were downright bizarre, such as recommendations for “internal fumigation”—otherwise known as blowing tobacco smoke through a tube up the butt.
From there, the path to modern resuscitation took shape slowly and made more practical progress (like in Boehm’s and Maass’s case). In the 20th century, accidents during surgery called for new ways of reviving the “apparently” dead, this time from the inside. In 1947, Claude Beck, an American surgeon, restored a heartbeat by using a defibrillator to shock an exposed human heart. He was also an advocate for the widespread use of open-heart massage, a common way to resuscitate people from surgical errors at the time.
Beck “kind of pisses off the conventional medical establishment by advising that people just carry scalpels, and then if somebody keels over, you just cut them open and you massage the heart,” said Gainty.
Luckily, others won out over Beck. Eventually, CPR became something anyone could learn to do, no scalpel required. While at Baltimore City Hospital, the late anesthesiologist Peter Safar pioneered the “ABCs” of CPR—airway, breathing, and circulation/compression. Though mouth-to-mouth resuscitation had been documented as early as the 1730s, Safar’s research made it a recognized part of CPR, showing that if you tilted someone’s head back in the right way (opening the airway), people could get enough oxygen to survive from only these “rescue breaths” for quite a while. (He did this by recruiting volunteers who agreed to be sedated, paralyzed, and given mouth-to-mouth. Yes, really.)

Mouth-to-mouth ventilation on Felix Steichen, one of Safar’s first volunteers for resuscitation research, in 1957.
Courtesy University of Pittsburgh/Peter SafarAt the same time, doctors succeeded for the first time in restoring a normal rhythm to a heart experiencing atrial fibrillation, which causes it to quiver uncontrollably. At the University of Pittsburgh, Safar established the first intensive care unit (ICU) in the United States in 1958. Doctors were getting better than ever at rescuing people from the brink of death.
And they still are. Today, doctors can keep people alive who would have surely died fifty years ago, including trauma patients—people who are severely injured and have very little blood left in their bodies and cannot be saved by mere CPR or other measures.
To buy time for these patients to be resuscitated, doctors began “working out the ability to allow an hour or two to have no blood flow,” Samuel Tisherman, a professor of surgery in the program in trauma at the University of Maryland School of Medicine, told The Daily Beast. Tisherman used to work with Safar to research the effects of inducing mild hypothermia—decreasing body temperature to around 90 to 92 degrees Fahrenheit from its original 98.6 F—in people undergoing cardiac arrest not caused by a traumatic injury.
The pair learned, partly through studies on dogs, that for those in a comatose state after cardiac arrest, lowering the body’s temperature by a few degrees during recovery seemed to decrease brain damage and boost the chances of regaining consciousness and recovering more fully. It’s not totally clear why, but the researchers suspect slowing down the body’s normal processes through lower temperatures helps to lessen brain injury associated with renewed blood circulation to the brain and other organs.
Tisherman is currently examining hypothermia induction through a more audacious clinical trial, decreasing body temperature down to 50 to 60 degrees Fahrenheit. After inducing hypothermia by giving the patient cold IV fluids, the doctors can perform surgery. Afterward, patients are put on a heart-lung machine, which restores blood and oxygen circulation to the organs, acting as a replacement for their heart and lungs, since the extremely cold body temperature has caused the heart to stop beating. With the body’s temperatures cut down much more drastically and its physiological processes substantially slowed down, surgeons have more time to address injuries and stop severe bleeding while worrying less about the patient’s injuries or the surgery causing significant damage to the body or brain. Afterward, the patient is transferred to an ICU where they can be warmed up and given new blood.
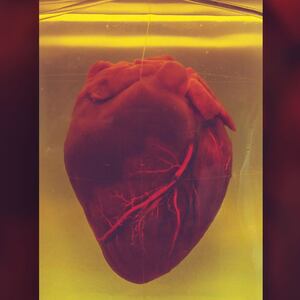
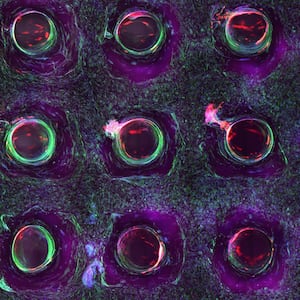
Which brings us to that pig study from earlier this year. You know the one. As organ shortages continue to leave patients in need in the lurch, researchers have sought new solutions that could help save lives. Back in August, researchers at Yale University announced a breakthrough: using an organ perfusion technology called OrganEx, which artificially circulates blood and fluid to dead organs, using a special fluid containing vitamins, minerals, and over 13 drugs in order to restore some cellular and organ function in a dead pig.
Though OrganEx incorporates a machine similar to a heart-lung machine, it’s descended from research in a different field, where doctors have come up with ways to use organs from dead patients for transplants—a practice called “donation after circulatory death.” The new demonstration broke open the potential for doctors to one day access a much bigger pool of organ donations that could save the lives of many more patients who are on the recipient list.
Of course, utilizing a “dead” organ, or one from someone who has died, is very different from reviving a seemingly dead person. The Yale researchers themselves who authored the OrganEx study told IEEE Spectrum in August they don’t view their research as redefining death—rather, they are simply developing new tools for cell and organ recovery. Likewise, doctors like Tisherman never view their patients being resuscitated as dead.
“If you stopped CPR while still in cardiac arrest, [the patient] would look dead,” Tisherman said. “There’s no pulse, there’s no breathing, there’s no brain activity.” But actually calling the patient clinically dead, while it might not be entirely inaccurate, he said, is misleading and confusing.
“The question is: Is it still reversible to the point of the patient surviving and being normal?” he said. “That's where resuscitation comes in.”
To doctors and researchers, death is a process, not an event. According to Gainty, the larger public used to share this perspective, back when humane societies tried to galvanize people to save the apparently dead. In some ways, she said, doctors and researchers are the victims of their own success.
In the 20th century, people started to see modern medicine as increasingly miraculous, bringing people back from the brink of death. Doctors have even helped reinforce this view. Beck, the same surgeon who once suggested that people might carry around scalpels and massage the hearts of people in cardiac arrest, once organized a “choir of the dead,” bringing together the first 11 people in modern medical history who were resuscitated and asking each, “How did you die?” Attitudes like his helped reinforce the idea that modern medicine not only could bring people back from the dead, but already had.
But even if death can be relative when it comes to organs—and in some cases—people, there’s no question—that Yale pig was dead. For hours. And though the researchers clearly didn’t bring it back to life, they also did something unprecedented, restoring organ function and even very limited brain activity. That’s especially significant considering that brain death has become our threshold of no return. You can put someone on life support, but once their brain activity stops, they’re gone.
Research to try to restore brain-dead people is, at this point, very limited, with little science to go on. The biotech startup Bioquark, whose clinical trials would have tested a way to do this, were stopped before they got started. The company’s “ReAnima Project” would have used a multi-step process, which included stem cell injections, a peptide formula injected into the spinal cord, nerve stimulation, and laser therapy, to try to promote recovery from brain death. The protocol was designed to mimic the process through which some amphibians, like salamanders, use to regenerate parts of their brain and nervous system.
“We got a lot of pushback,” Ira Pastor, formally the CEO of Bioquark and currently an independent biotech consultant, told The Daily Beast. He said many people in the neurointensivist world, including researchers and doctors who study and care for people with severe brain injuries, were angry that a small biotech startup would “try to do anything or even design a protocol for something that's been called irreversible.”
Charles Cox, a pediatric surgeon at the University of Texas Health Science Center at Houston who has worked with the same type of stem cells that were to be used in Bioquark’s trials, has put it a different way. Speaking about Bioquark’s protocol to STAT in 2017, he said, “I think the probability of that working is next to zero.”
Which is why any prospect of changing that, even a vague one, is a definite shift. “What happens if the kinds of experiments that were done with pigs’ brains begin to suggest that there might be ways we could resuscitate the brain?” Paul Root Wolpe, a bioethicist and director of the Center for Ethics at Emory University, said in an interview with The Daily Beast. As we are increasingly able to resuscitate people whose hearts have stopped and might have previously been considered dead, the cessation of brain activity has come to define death, said Wolpe. That line might be pushed back even further, he said, if brain death became something people could recover from.
For now, those questions are moot. We’re a far cry from any breakthrough that demonstrates anything close to recovery from brain death.
But if you can come back from death, were you ever really dead to begin with?
“One of the words that’s in the definition of brain death is the word irreversible,” said Wolpe. “Now we’re saying, wait a second, what if some of it’s reversible?”
This story is part of a series on the innovation of death—how research and technology is changing the way we put the deceased to rest, how we grieve, and how we perceive death moving forward. Read the other stories here: