Dr. Michael Salvana began to realize what kind of doctor he wanted to be on the third floor of a Post Office building in Cairo, Illinois. Fresh out of medical school in 1989, Salvana was stationed in the dilapidated city at the state’s southernmost tip through the National Health Service Corps, which footed the bill for his education. At the intersection of the Mississippi and Ohio rivers, developers had long ago eyed Cairo as the next big port town, but the city had been steadily abandoned by residents and government resources alike, leaving behind shuttered factories and boarded-up blocks.
By the time Salvana arrived, the only hospital in town was closed and vacant, so a community clinic set up shop above the Post Office. Salvana’s patients were some of the city’s poorest remaining residents, with complex medical issues that echoed the years of segregation, failures of local governance and blight left behind.
More than two decades later, Salvana was treating a similarly neglected population of patients, in another town with a borrowed name from a far-off city: Rome, New York. There, Salvana became the director of the Walsh Regional Medical Unit (RMU), housed in a medium security men’s prison and home to some of the state’s chronically ill prisoners.
Patients are sent to the Walsh RMU, one of the state’s five in-prison medical facilities, with an array of chronic and often terminal conditions: sickle cell anemia, late-stage cancer, multiple sclerosis, Parkinson’s, and severe spinal injuries are just a few of the ailments staff treat there. Many, if not most, patients suffer from chronic, excruciating pain. Salvana, who has specialized training in both pain and addiction treatment, saw relieving pain as central to his role, and he prided himself on lessening the suffering of his patients. But in June of 2017, that mission was abruptly interrupted. The New York Department of Corrections and Community Supervision (DOCCS) introduced a new policy that made it nearly impossible to prescribe the medications patients needed most.
The “Medications With Abuse Potential” policy (MWAP), penned by former Regional Medical Director David Dinello, was ostensibly written to address the abuse of opioids behind bars as the overdose crisis raged outside of prisons, according to both DOCCS and Dinello himself. Doctors throughout the state’s prison system were instructed to fill out the “MWAP” form, which required sign-off from regional medical directors, for a laundry list of medications to be prescribed—and providers rarely got what they asked for. The list wasn’t exclusive to opioids: Imodium, Claritin, Lyrica, Neurontin, and Gabapentin, a seizure-relief medication, were restricted alongside oxycodone, percocet, and Dilaudid. Doctors from prisons across the state, including Walsh, were instructed to wean their patients off of medications on the lengthy list, and were often denied requests for medications that had long proven effective for their severely ill patients by higher-ups who never examined them.
Walsh RMU, which was renovated in 2014 at a cost of $32 million to the state of New York, quickly became a nightmarish landscape of untreated pain and illness: epilepsy patients seized; sickle cell anemia patients went into crisis; men with late-stage cancer writhed; a Parkinson’s patient spasmed uncontrollably until falling out of his bed.
“When you went into their rooms you’d find these guys, grown men, in the fetal position rocking with pain,” said Salvana. “And you can’t give them their medication because someone 50 to 100 miles away who hasn’t seen them won’t sign a piece of paper.”
Some providers pushed back against the policy, emailing regional medical directors to decry the time-consuming process and their inability to treat patients who had long taken the restricted drugs without incident. Salvana was the most vocal, expressing outrage through emails, letters, and phone calls to Albany. Ultimately, he says, he was retaliated against and pushed out of his job—and now he’s suing the corrections department.
Prisons and jails are not the first choice of most medical practitioners looking for work. State correctional systems often struggle with chronic medical staff shortages, unable to recruit people to provide care in a less than desirable environment. Doctors and nurses who take jobs in corrections may intend to provide the best care possible, but they do so in the face of an ill-equipped system rife with apathy, understaffing, and budget cuts. As the incarcerated population ages, prisoners who are 55 years old and above comprise a growing segment, and prisons have struggled to deliver the nursing home-level care that is increasingly needed.
While credentialed, caring doctors and nurses do take these jobs, correctional facilities also have a well-earned reputation for attracting doctors who can’t find work elsewhere because of their own histories of misconduct or malpractice. This includes Dinello, who wrote and enforced the MWAP policy as a regional medical director for DOCCS. In 2010, the New York State Board for Professional Medical Conduct permanently prohibited Dinello from working in emergency medicine and ordered three years of probation, finding him guilty of professional misconduct during his employment at Auburn Memorial Hospital’s emergency room. Auburn cited three instances of Dinello failing to adequately examine patients before discharging them from the hospital in 2007 and 2008.
Dinello’s record of neglect and ongoing probationary period didn’t deter DOCCS, which hired him in 2009. His job remained safe when he pleaded guilty to misconduct in October 2010. By the time he wrote the MWAP policy and unveiled it to medical staff throughout the state’s prison system in 2017, Dinello—who did not respond to multiple requests for comment from The Daily Beast—was earning more than $180,000 per year.
Within a week of its introduction, the MWAP policy was angering providers and frustrating patients. Internal DOCCS emails obtained by The Daily Beast document frustrated back and forths between medical staff and the regional medical directors, including Dinello. In early June 2017, then-Deputy Superintendent of Healthcare at Walsh Amy Tousignant emailed Dinello to request Walsh RMU be exempt from the arduous policy:
“Providers are frustrated as what is being asked cannot be done in a timely manner…” she wrote. “Patients will suffer in pain and finally the nurses are being placed in a tough spot to address the medication needs not being met.”
A day later, Dinello defended his brainchild: “Unfortunately the Opiate Crisis is a Nationwide Epidemic and DOCCS is committed to limiting this disaster. There are 5 Providers at Walsh with a maximum patient load of 30 patients. Now is a good time to consider whether these patients truly need these Medications.”
One of those medications was Gabapentin, an anticonvulsant sold under the brand name Neurontin and often prescribed to people with epilepsy that also functions as a neuropathic pain reliever. Like many drugs, Gabapentin can be used to enhance a high if mixed with other drugs or taken in large quantities. Aware of this possible misuse, some DOCCS facilities were already administering it in liquid form to prevent abuse prior to the MWAP policy, calling into question how barring access to such a widely used pain reliever could prevent drug abuse. Further, incarcerated patients are highly surveilled and receive medications under close supervision, particularly in RMUs.
“This is an environment where they swallow it and you look in their mouth,” says Salvana. “You don’t give them a bottle of pills. These are patients who aren’t seeking out drugs for pleasure.”
Emails between providers and medical directors with MWAP forms show near-categorical denials of approval for Gabapentin and other restricted medications. Dinello frequently declined to approve medications that inmates had taken without incident for years. More than once, he denied requests for opioids by Salvana to treat a patient with sickle cell anemia, which had caused the disintegration of the prisoner’s hip and shoulder joints. Prior to the MWAP policy, like many people who live with sickle cell, the patient had taken opioids to manage pain for most of his life.
“There’s no ‘opioid crisis’ with a sickle cell patient,” Salvana says. “This is a medicine he needs for the rest of his life; there are physical reasons for this pain. There are some patients that need to be on drugs like this until they die.”
Dinello cited “Insufficient medical justification” for morphine to manage the patient’s pain, noting that “Opiate analgesia is reserved for Acute Pain Exacerbations unless the patient qualifies for End of Life or Hospice Care.” The patient was later air-lifted to a hospital in Albany in the midst of a pain crisis, where Salvana says he almost died.
In a review of MWAP requests, Dinello most often approved opioids or non-opioid medications for neuropathic pain for patients who were on their deathbeds, noting such meds were “more appropriate in DNR/hospice setting.” Even then, his approval was an uncertain bet: In August 2017, he declined to approve morphine for a patient with end-stage chronic obstructive pulmonary disease in need of palliative care.
The implication that incarcerated patients were chasing pain pills to get high — regardless of the offense they were incarcerated for, or how long ago they were convicted of a drug-related crime — was mostly implicit throughout the emails, though Dinello and other directors occasionally spelled it out.
In an email chain between three medical directors regarding a provider’s request for Neurontin in late 2017, Dr. Paula Bozer wrote from Eastern Correctional:
“It is amazing to me all the tricks that are pulled out of a hat in order to avoid stopping a controlled substance. If only all that intellect and conniving were put to better use...I think after workign [sic] for a long time in corrections, you develop an ‘inmate’ mentality: how can we circumvent the system and not comply?”
Alone in his prison cell with a baggie of heroin, Joseph Perez felt he had run out of options. "It was not something I wanted to do," Perez told me by phone in March. "I had tried everything I could to get [medical staff] to give me something to relieve the pain...it was falling on deaf ears. I was desperate."
Perez’s discomfort was visible to fellow prisoners at Five Points Correctional in Romulus, New York, and it wasn’t long before someone offered him a solution. Having virtually no experience using opioids, Perez immediately overdosed, but was revived with Narcan by a corrections officer. Largely using a wheelchair, he lives with chronic spinal pain following a motorcycle accident that occurred shortly before he was locked up in 2003 for robbery and burglary. From the time he entered prison until 2017, the medical staff working for the DOCCS administered opioids including oxy and percocet to manage his pain. But the MWAP policy abruptly cut off access to the one thing that helped him get through the day.
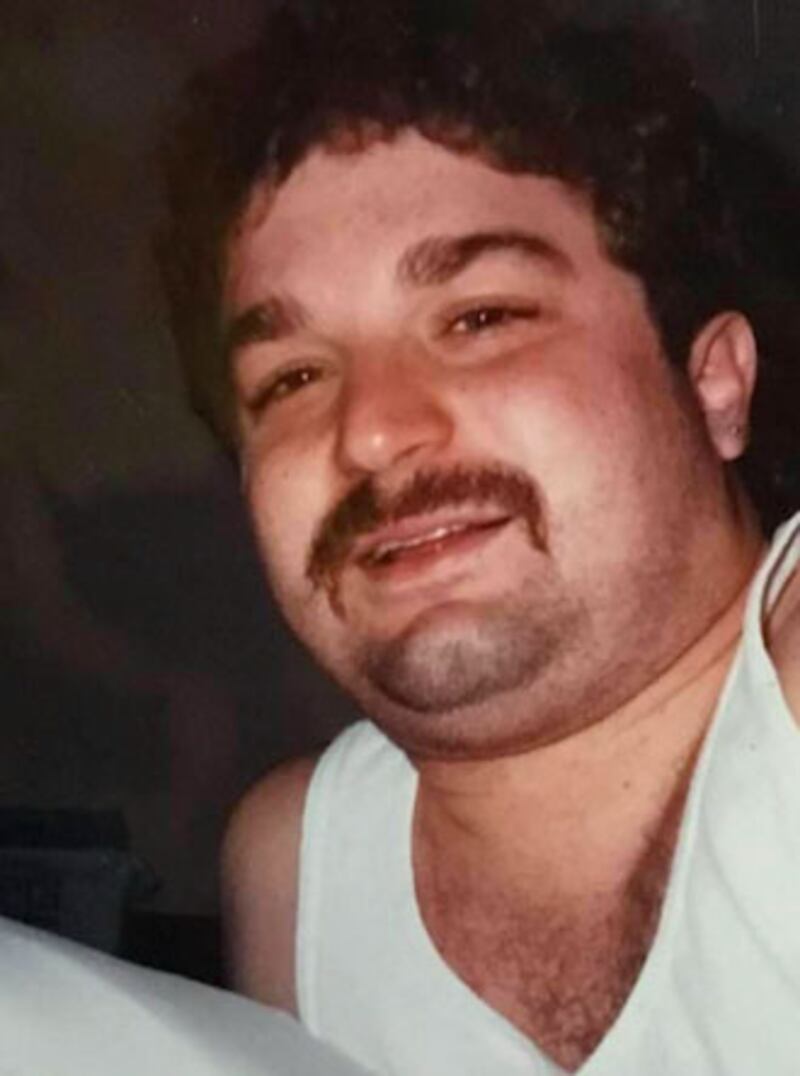
Joseph Perez
c/o John Perez“I went through all the motions of grievances and, writing to Albany, practically crying to the nurses, telling them I’m in pain,” said Perez. “All that didn’t get me nowhere.”
Perez isn’t proud of his choice to buy heroin, but says his pain was so extreme by mid-2018 that he was contemplating suicide. He experienced withdrawal after being taken off opioids over a very short period of time, and struggled to sleep or even use the bathroom without pain. Seeking relief became an all-consuming occupation. “It would’ve never come to that if I'd had my medication,” Perez adds.
Perez is a putative class member in a lawsuit challenging the MWAP policy, one of hundreds of men, filed by attorney Amy Jane Agnew in September 2019. After successfully suing DOCCS four years earlier on behalf of Anthony Medina, a blind prisoner who was denied pain medications, letters from prisoners across New York state describing similar situations came rolling in.
Agnew met with several letter-writers incarcerated at Shawangunk prison, including Aaron Dockery, a 35-year-old man with multiple sclerosis who described going from playing basketball while receiving Neurontin to requiring use of a wheelchair around the clock after MWAP was introduced.
“You’ve just mandated that a man spend his life in a wheelchair because you won’t give him a 50 cent drug,” said Agnew. “I remember meeting with these guys at Shawangunk and just thinking, ‘This is awful, this is unacceptable and can’t go on.’”

Aaron Dockery and his daughter
c/o Vyolet CirkoAgnew and her team identified an initial group of 18 incarcerated men whose meds were cut off, including Dockery, who they allege represent a larger putative class of hundreds whose Eighth Amendment rights to be spared cruel and unusual punishment were violated. The suit targets not only DOCCS, but former and current DOCCS providers. After months of depositions, discovery, and filings, DOCCS rescinded the MWAP policy in February of 2021 and replaced it with an amended version that placed the power to prescribe back in the hands of providers, rather than their higher-ups. Dinello resigned in early April.
“The policy, which no longer exists, is part of ongoing litigation and the Department has no comment,” DOCCS told The Daily Beast.
Agnew begs to differ. Though the letter of the policy has technically been revoked, she says, “They’re still doing whatever they want.” Though some of her clients, including Joseph Perez, have been reassessed by medical staff since the policy was revoked and are once again receiving pain relief medications, the process has moved at a glacial pace. She estimates that as many as 600 people are still without the meds they need, including severely ill patients in RMUs who are less likely to be able to advocate for themselves.
“DOCCS has not adopted any programs to fix this systemically,” says Agnew. “They’re just playing whack-a-mole for the litigation. What that means is that I’m driving health care. That’s not right. That’s crazy.”
As Agnew filed her suit, Salvana was fighting to preserve what was left of his job. After repeatedly pleading with Dinello and other regional medical directors to let him treat his patients, reaching out to DOCCS Commissioner Anthony Annucci, and calling other stakeholders in Albany, Salvana found himself increasingly isolated at work. Several other providers who raised similar concerns resigned and those who remained began to ice him out. Salvana’s lawsuit alleges that nurses under his supervision began to cancel his orders, and locked him out of critically ill patients’ rooms.
Unable to examine his patients or treat their pain and harassed by his colleagues, Salvana resigned in April of 2020. He is now seeking work outside of New York.
“I’m going to be 72 in a couple of weeks, and I don't like being in a retirement situation,” Salvana told The Daily Beast. “I want to die with a stethoscope around my neck. That’s how much I like medicine… I like what I do, and I like this population of patients.”
The crisis of un- or under-treated pain experienced by prisoners in New York echoes a problem faced by many chronically ill patients who aren’t locked up. In 2016, the CDC revised its opioid prescribing guidelines for primary care providers treating chronic pain. In essence, the CDC urged providers to exhaust all other pain relief options before turning to opioids, and to keep dosages extremely low when necessary. The following year, the same year DOCCS rolled out the MWAP policy, the Department of Health and Human Services declared the opioid epidemic a public health emergency.
The CDC guidelines were followed by a cascade of state, federal, and local efforts aimed at curtailing prescriptions to opioid pain pills; criminalizing sellers, users, and perceived over-prescribers; and efforts to punish major players in the pharmaceutical industry. Efforts were also made to invest in pain treatment research, substance use treatment, and education. Still, the scourge of prescription pills largely took center stage in the rush to try and stem the swell of addiction and death.
The CDC guidelines were also met with outrage from patient advocates, doctors, and many in the vast community of people living with chronic pain who rely on opioids to make daily life tolerable. Implicit in much of the broader anti-opioid dialogue and the policies that spring from it is a familiar suggestion that people who rely on opioids are out-of-control addicts, drug seekers and criminals who masquerade their fraudulent pain to get high. Perhaps nowhere is that mentality more omnipresent than in prisons and jails, where questioning and doubting the legitimacy of pain in the context of criminality, regardless of physical condition or offense, is commonplace.
The CDC’s recommendations were also followed by more overdose deaths: nationwide, more than 93,000 people died of a drug overdose in 2020, according to new CDC data. As prescriptions were tapered or cut off, many—like Joseph Perez—turned to street-based options like heroin, which is increasingly cut with Fentanyl, often with lethal results.
In a July letter, the American Medical Association urged the CDC to “remove arbitrary thresholds, restore balance and support comprehensive, compassionate care” when revising its guidelines, which the agency says will be released later this year. The chairman of the AMA Board of Trustees, Dr. Bobby Mukkamala, noted that the “threshold recommendations continue to be used against patients with pain to deny care. We know that this has harmed patients with cancer, sickle cell disease, and those in hospice. The restrictive policies also fail patients who are stable on long-term opioid therapy.”
Denying care in a prison can also reflect a darker truth: Some people’s pain simply matters less to people in power, or is perceived as part of an earned punishment.
“We get to punish people, but living in prison is the punishment. Being in chronic pain is not the punishment,” says Agnew. “We do not get to torture them. It’s that simple.”


