Millions of people around the world are in need of a major organ transplant, but very few are likely to find a viable donor. Over 106,000 Americans await a new organ, and 17 people die each day as they wait for a transplant. This is especially true during COVID, where the disease has decimated the respiratory health of thousands and left their lungs ravaged. A growing number of people are in need of a lung transplant—but there are simply too few lungs to go around to save everyone.
One of the biggest hurdles to transplantation is also a deceptively simple one: matching blood type. This is especially true for the heart and lungs, which are more sensitive than other organs to mismatched blood type, said Dr. Alexander Krupnick, a lung transplant surgeon at the University of Maryland Medical Center.
But new research out of Canada promises to solve this incompatibility obstacle by doing something quite extraordinary: converting the native blood type of an organ to a universal blood type.
In a new study published on Wednesday in Science Translation Medicine, Toronto researchers were able to take donated lungs and strip them of the antigens that identify them as blood type A, making the lungs appear as if they originated from an individual with blood type O donor—famously known as the universal donor blood type. (Though technically, O-negative is the true universal donor type.)
The research team behind the new paper achieved this breakthrough by flooding the donated blood type A lungs with two enzymes that can remove blood type A antigens from cells lining the organ’s blood vessels, where most of the troublesome blood type incompatibilities manifest. Within about four hours, the enzymes—called FpGalNac deacetylase and FpGalactosaminidase, and naturally produced by our bodies—removed more than 97 percent of type A antigens from the donated organs.
The team then tested out the lungs to see whether or not they would lead to a phenomenon called hyperacute rejection, which happens when a recipient is given the wrong blood type.

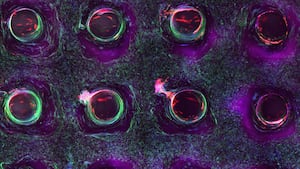
Dr. Aizhou Wang demonstrates the enzymes delivery to an Ex Vivo Lung Perfusion (EVLP) system,
University Health Network“We basically took two lungs from the same donor,” Dr. Marcelo Cypel, surgical director of the Ajmera Transplant Center and a co-author of the new study, told The Daily Beast. “The right lung we treated with enzymes, and the left lung we didn’t treat with enzymes. And then we put blood in both of them from [type] O donors. We could see the left lung performed stable [with] no signs of hyperacute rejection, while the other [showed] signs of hyperacute rejection very clearly.”
Cells treated with these enzymes will regenerate type A antigens over time, so this new approach is not a permanent and wholesale way to convert an organ to a new blood type. But it does alleviate some of the immunological obstacles that lie in wait during a patient’s first week after transplant surgery.
“If you put an organ in somebody and you don’t give them enough immunosuppression, the organ is rejected within a week due to antibodies,” said Krupnick, who was not involved with the new study.“This [research] is the step in the right direction of modifying the immunologic nature of organs. This is one step in what could be multiple steps to take any organ and put it into any person with the need for lower amounts of immunosuppression.”
Beyond erasing a donated organ of its blood type, Krupnick said the method could be used to address another thorn in the side of transplant medicine. There’s a group of genes involved in how our immune systems recognize native and foreign proteins and pathogens, called the major histocompatibility complex (MHC). The antigens produced by these genes account for the differences in immunity within a population, like why some individuals succumb to COVID-19 and others show no symptoms at all. And the MHC can create obstacles when trying to match donors with recipients.
“If you strip some these [MHC] antigens, and you put the organ, and if the antigens come back in a couple of weeks, your body reacts much less to the organ” than when it initially is transplanted, because your immune system is more sensitive in the first week, said Krupnick. The enzymes could provide a path for doctors to learn how to temper down the MHC antigens for new organ recipients.
The new findings arrive at a time when organ transplant research has taken some huge steps forward. In January, a Maryland man underwent the first-ever successful pig-to-human heart transplant. Later that month, surgeons at the University of Alabama in Birmingham successfully transplanted a pig kidney into the abdomen of a brain-dead man. These breakthroughs in animal-to-human transplantation are a very different approach to solving the organ transplant shortage, but they will still require a lot of development before we might see them used as a regular solution to organ transplants. For now, modulating existing organs could be an easier way to make do with the organs that are actually available.
Cypel said the next research stage is to test out his group’s findings in mice studies and investigate the kidneys as a next target organ, which is one of the top organs in demand with over 90,000 patients waiting for a kidney transplant.
“We still need to do studies before we can say that it could be used in clinical practice,” Cypel said. “But when we get to that point, you know, this could transform the way we allocate organs.”