As infections go, Jeffrey Siegelman’s first bout with COVID was unremarkable. The emergency physician and professor at Emory School of Medicine likely contracted the virus while on the job in August 2020. He experienced the usual symptoms—fever, headaches, aches, chills, and loss of smell and taste. But in the weeks after he recovered, other symptoms set in, including heart palpitations, insomnia, and significant fatigue after even minor physical exertion. The headaches also never went away, he said.
“Here we are two years later, and I'm still dealing with a lot of that stuff,” Siegelman told The Daily Beast.
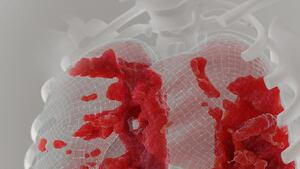
Tens of millions of Americans, Siegelman included, are suffering with the after-effects of a COVID infection. Long COVID, defined by the Centers for Disease Control and Prevention, represents “a wide range of new, returning, or ongoing health problems” that people experience weeks after being infected with the virus. A new study, published Wednesday in The Lancet Psychiatry, measured the range of ongoing neurological and psychiatric symptoms that over a million people faced after a diagnosed COVID infection, and compared them to people who contracted any other respiratory virus.
The biggest takeaway is that these neurological and psychiatric symptoms can linger for at least two years after infection in some people. But the results have to do with more than just COVID—according to the authors, they underscore the need for a new and thorough commitment to mental health infrastructure to support increasingly strained health care systems.
“It's well-established that adults, in the few months after diagnosis of COVID-19, are at an increased risk of a range of neurological and psychiatric conditions,” lead study author Maxime Taquet, an Oxford University psychiatry researcher, said during a press briefing. “There's quite a few questions that remain unanswered, and the first one is what happens after six months.”
The researchers analyzed the health records of nearly 1.5 million patients diagnosed with COVID, and matched them with other respiratory illness patients based on variables including age, sociodemographics, and risk factors. Then they determined if members from each group were diagnosed with any of some 14 psychiatric or neurological disorders, and when. These conditions ranged from anxiety and mood disorders to insomnia to dementia—according to Oxford psychiatric neuroscientist and study co-author Paul Harrison, these conditions are “intersecting with the long COVID story” but do not capture the full range of symptoms reported by patients.
For some of the conditions the researchers studied—including anxiety and mood disorder, stroke, and insomnia—COVID patients’ risks started out higher but decreased over the course of the two years and became similar to the people who contracted other respiratory illnesses. This finding is “very reassuring,” Taquet said.
But on the flip side, the risk of other disorders—including brain fog, dementia, psychotic disorders, and epilepsy and seizures—can remain high even after those two years. The researchers found that, compared to the other respiratory infection patients, more new cases of these conditions were still being diagnosed in people two years after a COVID infection.
The researchers also compared the diagnosis rates of these conditions among patients infected with alpha, delta, and omicron variants of the virus. They found that the emergence of the delta variant corresponded to an increased risk of neurological and psychiatric diagnoses.
Still, the risks between delta and omicron were largely similar—leading the authors to conclude that “health services will likely continue to face a similar rate of these post COVID-19 diagnoses even with SARS-CoV-2 variants that lead to otherwise less severe disease.”
Siegelman said that there’s a misconception that long COVID is actually depression or anxiety, and that the virus can’t possibly be causing long-lasting physical symptoms. The new study “argues pretty strongly that it's not,” and that these symptoms can last for years or longer, he said.
Though the study was large and tracked people over a comparably long period of time, the researchers said there were several limitations on its generalizability. For one, using electronic health records and confirmed COVID diagnoses restricted their sample to people who may have had easier access to health care or a more severe course of infection. In particular, the reliance on health records may have excluded communities of color, who are underrepresented in both research and medical care, Siegelman said.
Even Taquet’s own experience underscores this point: “There are people who have had COVID-19, including myself, who did not seek medical attention and therefore that would not feature in their health records,” he said.
Relying on electronic health record data also prevented the researchers from comparing rates of conditions based on disease severity or vaccination status, and the study does not explain how and why COVID leads to an increased risk of neurological and psychiatric diagnoses. Ongoing research is underway by labs all over the world to address these questions.
While an associated essay in The Lancet Psychiatry called for further investigation by forward-looking, prospective studies, Siegelman said that it’s not too soon to start taking action to help people with long COVID, as a clinician and patient himself.
“I think there's enough evidence here that there's a large group of people that have been infected, that are still suffering, and they deserve attention,” he said.