Shortages of personal protective equipment in some New York City medical facilities have grown so dire that health-care professionals are bucking directives from their executives to reuse gear and making an end-run at Governor Andrew Cuomo’s office to plead for additional supplies.
Over the past two weeks, a handful of New York health-care executives told state representatives—including those in Cuomo’s office—that they were not running low on personal protective equipment (PPE) because they implemented protocols directing staff to reuse items like face masks and gowns when treating COVID-19 patients, according to three individuals familiar with the conversations. Executives said they drafted those protocols, which include sanitization of personal protective gear, based on guidance from the Centers for Disease Control and Prevention (CDC), those sources said.
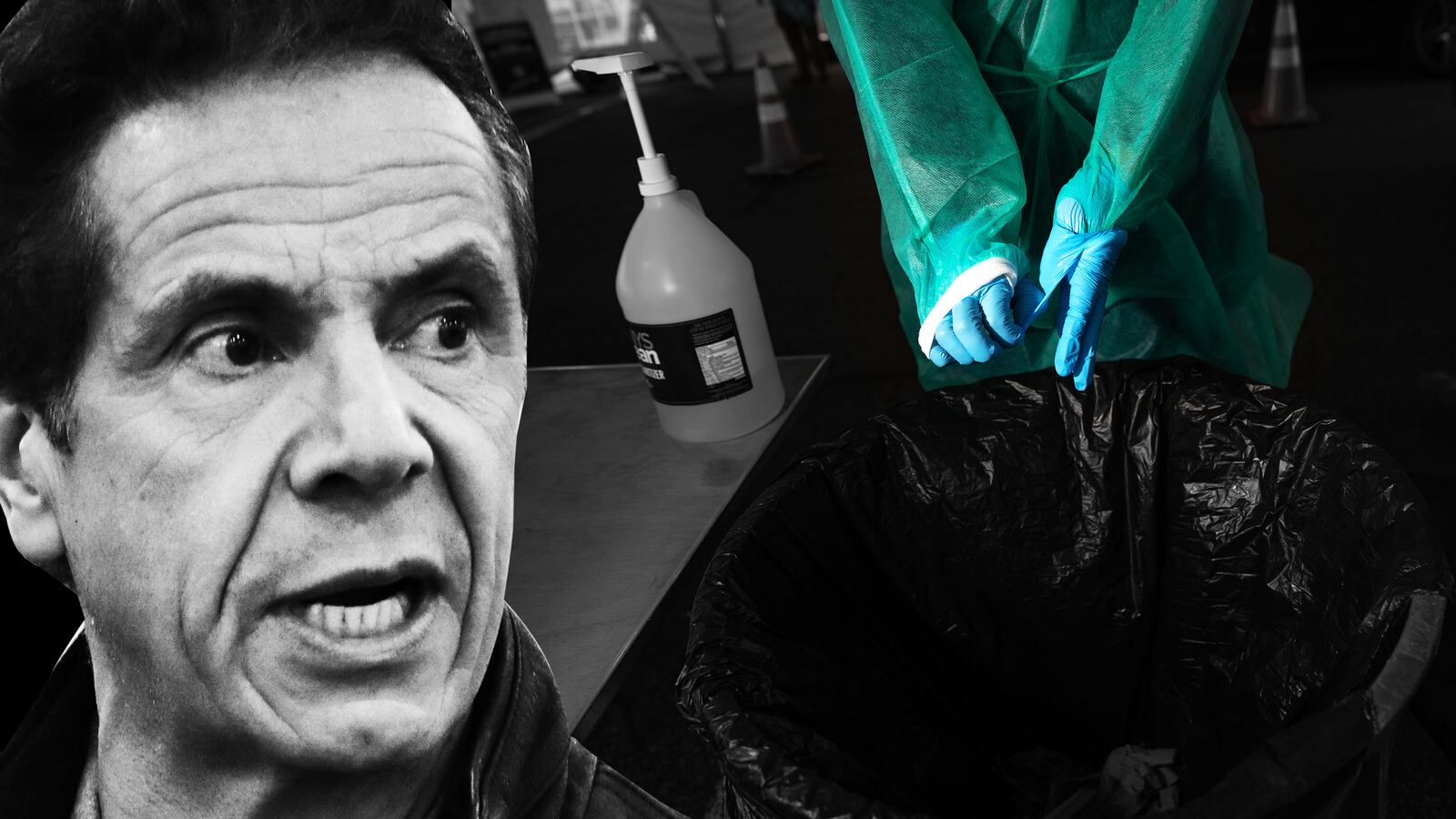
But the lack of protective gear and the restrictions on the stockpiles have forced some health-care professionals in the city to resort to wearing trash bags over their scrubs to imitate medical gowns. Doctors and nurses are at times forced to wear makeshift face shields to preserve the heavy-duty ones.
Now, medical workers are reaching out directly to state officials, including Governor Cuomo, to ask for help.
“There’s this idea out there that everything is fine and we all have what we need, but that really isn’t the case,” said one nurse who spoke to The Daily Beast anonymously because they did not want to lose their job. “We took on the job of calling the governor’s office ourselves and letting them know the situation we were in.”
The conversations come as the number of coronavirus cases continues to spike in New York. In a 24-hour period ending Monday, almost 7,000 people in the state tested positive for the virus, and 253 people died. The calls to the governor’s office by doctors and nurses about the shortages of protective gear underscore the severity of the situation, particularly in New York City, where some hospitals last week set up makeshift morgues.
Despite the cries for more equipment from health-care professionals across the country, particularly in hotspot regions, President Donald Trump has pushed back on the idea that states are in need. In an interview with Fox News Monday morning, the president said he was not worried about reports of protective gear shortages. “New York should be fine,” Trump said. “Based on the numbers that we see, they have more than enough.”
Cuomo, too, has at least tried to ease fears about medical supply shortages, saying in a press conference last week that “no hospital, no nurse, no doctor can say—legitimately—‘I don’t have protective equipment.’” Cuomo has since walked back that statement and said his government was working on obtaining more gear through donations and both U.S. and international purchases.
When asked for comment on the medical workers’ calls to the governor, his office pointed The Daily Beast to his statements to the press on Monday morning.
“The doctors are exactly right,” Cuomo told reporters at a briefing, adding, “We respect them and we love them for what they’re doing. They should have every piece of equipment that they need to do their job. That is the least that we can do. We are all doing everything we can to make that a reality.”
But medical workers still don’t have the gear they need, according to six health-care professionals working in New York City who spoke to The Daily Beast for this story.
Shanna Herron, a medical professional at a Queens-based nursing home, said nurses at the facility were wearing trash bags at gowns over the weekend after being told by administrators that there was not enough to go around.
Herron said the facility had previously experienced a coronavirus outbreak on the floors that house short-term patients and that one individual residing in the long-term care ward tested positive last week.
“It’s starting to spread,” Herron said. “And every day the protocols are changing. There’s been little communication from the top down on how we’re supposed to handle things. Usually we just find an email or a notice on the desk that tells us what to do.” Herron did say that administrators told her last week the facility had received a shipment with new gear, including gowns. “But all of that is still sitting downstairs,” she said. “It has to be brought up and distributed.”
The nursing home facility is also experiencing an uptick in the number of nurses leaving their jobs, some citing the lack of proper personal protective equipment and restricted distribution, Herron said. “At one point we had 40 patients to one nurse,” Herron said. “That isn’t safe.”
A doctor at NYU-Langone who treats coronavirus patients on a daily basis said his hospital has been reusing equipment for weeks while administrators stockpile for another bump in coronavirus cases.
“The masks aren’t on the floor anymore,” the doctor told The Daily Beast on condition of anonymity so he could speak freely on the topic. “You have to go and ask for it and then someone will unlock the cabinet for you.”
Several hospitals in New York are advising staffers to disinfect their protective gear before it is used again.
“NYU Langone Health has appropriate levels of PPE. But ... we are doing our very best to conserve its use so that it can sustain us through the duration of this crisis,” a spokesperson for NYU Langone Health said. “We are asking staff to re-use PPE according to CDC guidelines. We also are continuously educating our staff to the appropriate use of PPE, such as who needs to utilize what PPE in each clinical setting.”
On its website, the CDC has said hospitals should implement programs for the rationing of personal protective gear in times of shortages. Hospitals should include “provisions for the cleaning, disinfecting, inspection, repair, and storage of respirators used by workers on the job,” the CDC says.
In at least two hospitals in Manhattan, administrators are considering implementing a protocol that would advise health-care workers to put on one set of personal protective gear at the beginning of the shift and keep it on throughout the day, according to two doctors who spoke with The Daily Beast.
But health-care workers aren’t convinced. And medical experts caution against the wide-scale implementation of reuse protocols without proper data collection on whether techniques like sterilization actually work.
“Six weeks ago, nobody would’ve suggested reusing face masks and other PPE,” said Irwin Redlener, director of the National Center for Disaster Preparedness at Columbia University and an expert on U.S. readiness for pandemics. “We’re now operating in the climate of crisis standards of care. It’s already started, and it’s something that we’ve always feared.”
Redlener said the idea of sterilizing and reusing personal protective gear is not out of the question. “It’s just a matter of testing,” he said, explaining that the CDC should test various sterilization techniques on gear to determine what is safe to reuse.
The federal government is working with the clothing company Hanes to develop a cloth face mask that “meets the standards for protection of hospital workers but could be washed and reused,” Redlener said.
Dr. William Haseltine, president of the global health think tank ACCESS Health International, who recently chaired the U.S.-China Health Summit in Wuhan, said that other countries—including India and Peru—do reuse medical equipment, including N95 masks.
“I believe it can be done, but it should be done in ways that are controlled and are approved,” Haseltine said. “It shouldn’t be done fly-by-night or in the unapproved protocol. The whole purpose of regulation is to show that there’s assurance they will be safe.”
Dr. Timothy Brewer, a professor of epidemiology and medicine at UCLA who has served as an adviser for the World Health Organization, CDC, and National Institutes of Health, said he and his colleagues who practiced medicine in Peru often reused N95 respirators.
“That’s obviously not how we use them in the United States, but it’s better than not having anything at all,” said Brewer. “We’re now in a situation where we have to be more judicious in their use and probably have to reuse them in order to have access to them while we’re caring for COVID patients.”
But Brewer noted that the most important next steps involve the production of new masks and streamlining the process of reuse. Sterilization, he said, could involve chemicals that break down the materials in the mask, damaging their effectiveness, and—without data on which processes are safe—the focus at the moment should be on maintaining good hand hygiene and caution when taking masks on or off.
Ultimately, said Brewer, “we have no data in the U.S. that I’m aware of” on whether it is safe to reuse the masks.
“My colleagues in other countries felt it was better than not having a mask at all, and I would agree with that,” he added.