Parkinson’s disease has a list of recognizable symptoms, including tremors, loss of smell, and confusion. But the standard method of diagnosing the condition is nowhere near perfect: It classifies a patient's symptoms into supporting, excluding, or “red flag” criteria and makes a deliberation based on the presence (or absence) of each.
What this means is that patients who have Parkinson’s disease may go through life not knowing they have it, and patients diagnosed with Parkinson’s may actually have a different condition.
A team of neuroscientists from The Hebrew University of Jerusalem have just developed a new method to diagnose early-stage Parkinson’s disease that relies on brain scans instead of behavioral symptoms. Published Friday in the journal Science Advances, the new method could help doctors diagnose the disease earlier and with more certainty, and unlock a deeper understanding of the neurological changes caused by Parkinson’s.
ADVERTISEMENT
“What we have discovered is the tip of the iceberg,” senior author and neuroscientist Aviv Mezer said in a press release.
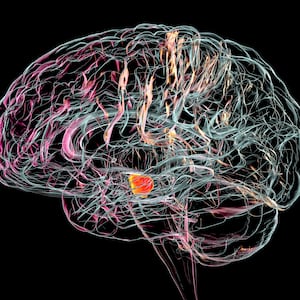
The researchers used brain imaging data called quantitative MRI scans to investigate small-scale changes in the striatum (a region of the brain that controls decision-making) that might be due to Parkinson’s. First, they collected data for healthy older and younger adults to see how aging alone might affect the striatum; then they expanded their sample to a clinical dataset of Parkinson’s disease patients. They also developed an algorithm to analyze the quantitative MRI scans automatically, allowing them to process scans of over 100 people.
Typical aging, they found, caused small-scale changes to multiple parts of the striatum, but early-stage Parkinson’s had a distinctive effect on the posterior segments of the putamen, an area on the back of the striatum. Some of these changes corresponded to lower dopamine levels and severity of motor symptoms for the patients—two key Parkinson’s symptoms.
Future work is needed to verify the team’s results in larger groups of people. According to the press release, Mezer is developing this application of quantitative MRI into a clinical tool. Being able to peer into the brain could allow researchers to separate Parkinson’s patients into subgroups and test drugs that have a higher chance of working. Other applications might include using the tool to diagnose other neurological conditions, like Huntington’s disease, the authors wrote in the study.