Last week, the World Health Organization came out against remdesivir, one of the most popular antiviral therapies for COVID-19, threatening to blow up some clinical practices in the United States. “I’ve no idea how to approach this,” Yogen Kanthi, a cardiologist at the Northville Health Center in Michigan, told The Daily Beast.
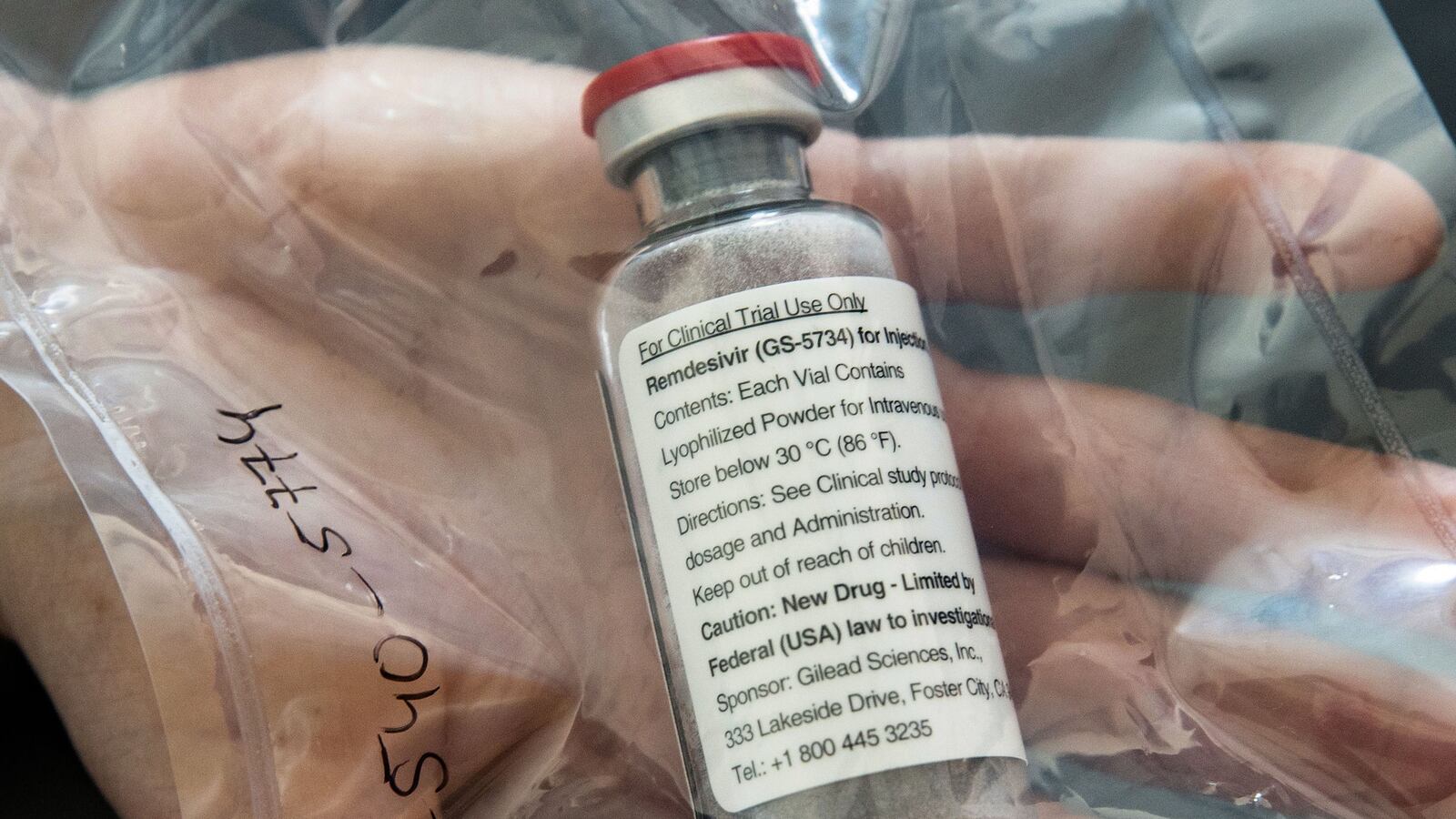
Many doctors stand by remdesivir, a product of California pharma Gilead originally designed to treat hepatitis C. The WHO’s stance, they argue, was based on a relatively low-quality survey of the drug’s effectiveness, and Gilead has called the agency’s position “disappointing.” But remdesivir’s popularity among U.S. clinicians as a COVID treatment is largely based on findings of modest effectiveness, and in poorer countries where medical resources are thin, the drug’s benefits might not justify its hefty price tag.
Welcome to Rabbit Hole, where we dive deep on the biggest story. It’s for Beast Inside members only. Join up today.
The WHO has stressed that its “conditional recommendation against the use of remdesivir in hospitalized patients,” announced Friday, was, in fact, “conditional.” In other words, views on remdesivir could change. And it seems unlikely most physicians in the United States are about to totally abandon remdesivir, which the WHO has no power to compel them to do.
Nine months into the novel coronavirus pandemic, many clinicians have settled on a course of treatment that includes remdesivir along with supplemental oxygen and, at a growing number of hospitals, new monoclonal antibody therapies. “Remdesivir is recognized as a standard of care for the treatment of hospitalized patients with COVID-19 in guidelines from numerous credible national organizations,” Gilead said in a statement after the WHO made its move.
It’s testament to how comfortable many doctors had gotten with their COVID treatments that the WHO’s blast against remdesivir caught some by surprise.
Irwin Redlener, the founding director of Columbia University’s National Center for Disaster Preparedness, described the WHO’s announcement as “weird.” Otto Yang, an expert in infectious diseases at UCLA, told The Daily Beast he was also skeptical. “It smells political and not evidence-based,” Yang said.
In fact, there was a process behind the WHO’s announcement, however controversial it might be. Starting in mid-October, the Geneva-based agency assigned 33 experts, including 28 clinicians, to sift through a variety of research into remdesivir. The experts examined results from four clinical trials, including one that the WHO itself organized.
Altogether, the four trials involved 7,000 COVID patients, around half of whom were treated with the Gilead antiviral. “There is currently no evidence that remdesivir improves survival and other outcomes in these patients,” a WHO spokesperson told The Daily Beast.
Some experts pushed back against the claim. “It seems to me this report is flying in face of what most clinicians believe to be the case,” Redlener said.
For months, the consensus in the United States has been that remdesivir, a broad-spectrum antiviral, helps to reduce the severity of COVID infections and speed the recovery of many hospitalized patients—although the drug doesn’t necessarily prevent the worst-off patients from dying of COVID.
A major study published in the authoritative New England Journal of Medicine on Nov. 5 supports that consensus.
Researchers divided 1,062 hospitalized COVID patients into roughly equal groups. One group got remdesivir. Another got a placebo. “Those who received remdesivir had a median recovery time of 10 days… as compared with 15 days… among those who received placebo,” the authors concluded. “The patients who received remdesivir were found to be more likely than those who received placebo to have clinical improvement at day 15.”
Overall, patients receiving remdesivir also had a slightly better survival rate than those in the placebo group. “Estimates of mortality were 6.7 percent with remdesivir and 11.9 percent with placebo by day 15 and 11.4 percent with remdesivir and 15.2 percent with placebo by day 29,” according to the study in NEJM.
Redlener called the NEJM study “extraordinarily credible.”
Keith Armitage, an expert in infectious diseases at University Hospitals in Cleveland, told The Daily Beast the trial which NEJM published the results of was more authoritative than the WHO study, which loosely combines different types of data from a variety of trials.
However, the NEJM study certainly doesn’t claim remdesivir is some kind of cure-all. Instead, it shows “a mild benefit” from the drug, Leila Hojat, another University Hospitals infectious-diseases expert, told The Daily Beast. “Remdesivir has never been touted to be an extremely powerful antiviral,” she added.
In a country as wealthy as the United States, mild benefit might justify the use of a fairly expensive drug. “We are willing to invest as many resources as needed for even a small benefit,” Hojat said.
But the WHO makes recommendations for health systems all over the world, including in very poor countries. “Given that many of these areas may be more resource-limited, it makes sense in their setting not to recommend that remdesivir be used routinely,” Hojat explained.
Asked whether remdesivir’s cost was a factor in the WHO’s rejection of the drug, a WHO spokesperson simply repeated the organization’s claim that it was ineffective against COVID-19.
Some U.S. clinicians were quick to shrug off the WHO’s recommendation.
“We always knew remdesivir had mild efficacy at best, but I am not sure I agree with [the] WHO decision to jettison it completely at this juncture,” Christopher King, a pulmonary and critical-care specialist with the Inova Medical Group in Virginia, told The Daily Beast.
For a few, however, the WHO’s assessment seemed to be helping to tip opinions against the drug. “Yes, the WHO may have gotten this right,” Shashank Sinha, a cardiologist with the Inova Medical Group, told The Daily Beast.
There’s just one thing all the experts The Daily Beast spoke to agreed on. They all want to see more trials involving remdesivir—even as the biotech world turns its collective gaze toward a vaccine.
“This is going to have to get resolved one way or another by additional reviews by other credible authorities,” Redlener said.