Much of the woes and struggles of starting a family center around women and their fertility issues. But for a third of all heterosexual couples grappling with infertility, the problem lies squarely with the man. Faulty sperm tends to be the No. 1 culprit. Around 10 percent of infertile men (and 1 percent of all men) suffer from azoospermia, a condition in which sperm is completely absent in the semen. While there are treatment options available, like medication or surgery, these methods aren’t an option for some men who can’t make sperm at all. So some scientists are instead turning to the world of 3D printing to solve azoospermia.
In a new study published March 16 in the journal Fertility and Sterility Science, Canadian researchers 3D-printed live and functional human testicular cells for the first time ever. This accomplishment likely lays the groundwork for solving sperm-associated forms of male infertility in the future.
Azoospermia comes in two forms—obstructive and non-obstructive. The former has a simple fix: Surgeons unblock or create the tubes that carry sperm from the testes out to the rest of the male reproductive system.
But with non-obstructive azoospermia—the most severe form of the condition—men aren't making sperm at all, and that could be due to many different reasons, some of which can be genetic like Klinefelter syndrome (where less testosterone is made because there’s an extra X chromosome) or hypogonadotropic hypogonadism (where puberty is delayed or completely absent). Solving this problem first required understanding what was happening deep down at the cellular level.
“We needed something as close to the nature within a testicle as possible to be able to study this as a functional unit,” Dr. Ryan Flannigan, a urologist at the University of British Columbia who led the new study, told The Daily Beast.
The new study started with Flannigan and his team growing testicular tissue in the lab and observing how this community of cells organized itself, communicated with each other, and responded to different growth hormones. They began to ask: Why not try regenerating a whole testicle, or at least a clump of testicular cells, with 3D printing?
To do that, they biopsied stem cells from the testicles of a 31-year-old man with non-obstructive azoospermia and grew as many new stem cells as they could in the lab. They then used these cells to 3D-print a structure similar to the seminiferous tubules, structures within the testes where sperm are born.
The researchers kept the seminiferous tubules nourished with the hormones, nutrients, and other chemicals they needed to stay happy and grow. After about two weeks, the cells flourished, much to Flannigan and his team’s surprise. While they didn't form single-and-ready-to-mingle sperm, they were able to advance into stages that are nearly partway through the multi-stepped creation process.
The next step, of course, is to get these 3D-printed testicular cells to make sperm. Once achieved, Flannigan is hopeful they can be used to help provide insight into treating male infertility. Doctors might even use them directly during assisted reproductive procedures like in vitro fertilization (IVF).
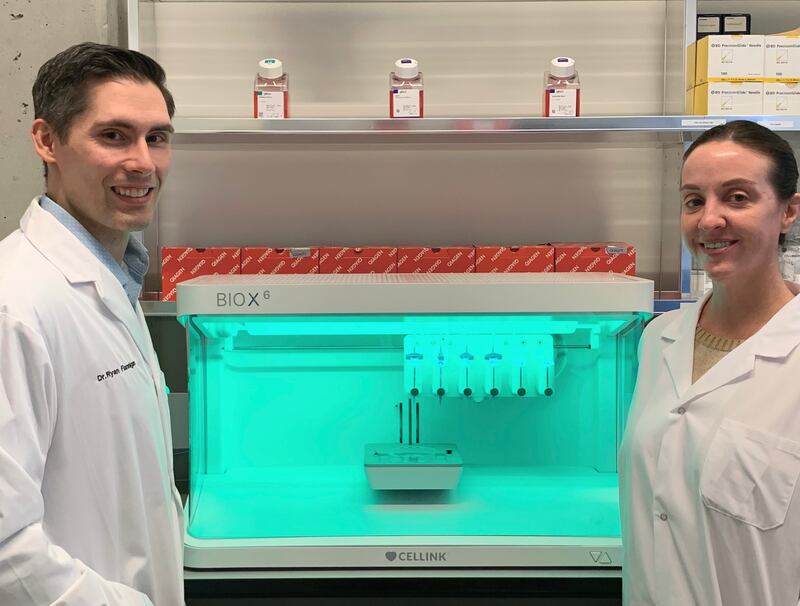
Ryan Flannigan and Meghan Robinson in front of the testicular cell 3D printer.
Courtesy University of British ColumbiaThese 3D printed cells might also be able to help male cancer patients preserve their fertility before undergoing aggressive treatment.
“Pediatric cancer patients who undergo chemotherapy or radiation therapy undergo that before they hit puberty,” said Flannigan. “Some of them will regenerate sperm if they recover from treatment and their testes recover. But a big proportion of them won't recover and won’t have any opportunities to have biological children of their own.”
While there’s no technology available yet to develop stem cells into fully mature, functional sperm, Flannigan said harvesting and freezing a cancer patient’s stem cells before treatment will at least give them a fighting chance for the future.
“The field of regenerative medicine and using approaches like this is probably going to have a bigger presence in the future,” he said. “It’s all fairly early on in development and there’s a lot of people doing parallel research in other organ and disease systems [but] it’s an exciting field to watch out for.”