Although vaccines greatly reduce the chances of a severe COVID-19 infection, “long COVID” is still a risk most people want to avoid. Some studies suggest that up to half of all people who have survived infection experience symptoms of long COVID, including tiredness, chest pains, difficulty breathing, sore joints, and a loss of taste or smell.
It’s been difficult to figure out who could be more susceptible to long COVID (also known as post-acute coronavirus disease syndrome, or PACS). But thanks to some immunological insights from a study run by Swiss researchers, doctors and patients alike might soon have a new tool to predict the likelihood someone will develop the condition.
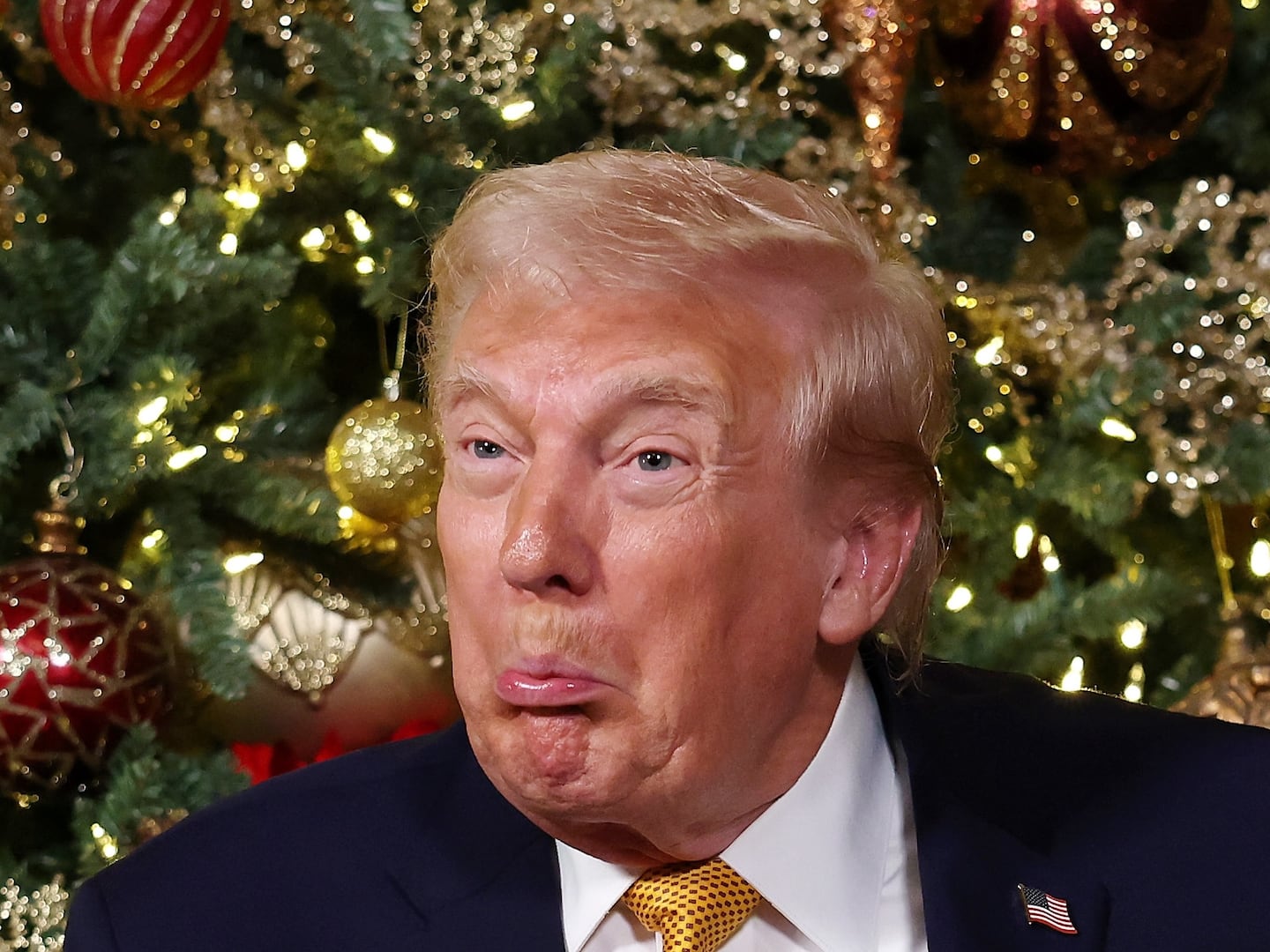
“It took some time until people realized what COVID-19 is and an even longer time to realize that a subset of COVID-19 patients did not recover from acute disease,” Onur Boyman, an immunologist at the University of Zurich and senior author of the new study, told The Daily Beast. “The symptoms experienced by patients with PACS can be very different and affect various organs. We are looking at a condition with different causes, making it more difficult to find relevant patterns to understand the disease.”
Published Tuesday in Nature Communications, the new findings are the first time scientists have identified how antibody levels differ between those who suffer long COVID and those who don’t. By combining the new data with a few risk factors, Boyman and his colleagues have developed a model that can calculate long COVID risk for any patient in the early stages of infection.
As part of the study, the researchers studied a cohort of 175 COVID patients and 40 healthy individuals for one year. Among the COVID cases, 53.9 percent of mild infections and 82.2 percent of severe infections led to long COVID symptoms.
In analyzing the blood of COVID cases, the research team found that PACS patients typically exhibited lower levels of two types of antibodies: IgM, which is important in early immune responses to infections; and IgG3. which plays a big role in combating viruses. These levels were stable over the course of the whole year, which means a blood sample taken at any point in time, regardless of infection status, always returned the same IgM and IgG3 results.

Onur Boyman
Thomas Buchwalder / University of ZurichBoyman and his team used the antibody data, along with risk factors like asthma and old age, to develop a predictive model that would score a person’s risk for COVID on a scale of 1 to 100. They tested the model out on another set of 395 COVID-19 patients. Though accuracy varied between groups and settings, Boyman and his team found the model was clinically useful in guiding treatment decisions for anyone whose PACS score was over 55.
The model is not yet ready to calculate risk before COVID infection strikes, since it uses symptom severity as part of its calculation. But nonetheless, “it should be possible to use [antibody] measurements obtained already prior to infection,” said Boyman. The Swiss researchers hope to improve the prediction model through further testing, including on patient cohorts outside of Central Europe. And eventually, they hope to find a way to predict long COVID based solely on blood work.
The research team is already in the process of developing an online tool that uses their new model to calculate long COVID risk in people. No answer yet for when it will be available, but if it passes muster through future testing, it could be an invaluable tool in helping deliver early treatment to patients to help prevent or mitigate long COVID—especially now that we’re increasingly on our way to seeing COVID become an endemic disease.