After decades of failed experiments and mixed results, a malaria vaccine has earned the endorsement of the World Health Organization. It’s a long-awaited tool to combat a disease that kills hundreds of thousands every year, mostly young children in sub-Saharan Africa.
On Wednesday, WHO officials gave their stamp of approval for Mosquirix, which has proved to be about 50 percent effective in preventing severe malaria in the first year of vaccination. The vaccine was in development for 30 years, finally achieving demonstrable success while countless other candidates petered out. Health experts and clinicians have faced an absolute grind to get to this point.
And the efficacy rate does highlight that the vaccine is far from perfect, Brian Grimberg, an associate professor of pathology and international health at Case Western Reserve University, told The Daily Beast. He suspects this endorsement probably happened because progress against malaria has stagnated in recent years.
“The WHO is saying: let’s try something, because we’ve stalled,” said Grimberg.
Malaria is both preventable and curable, and the developed world remains quite insulated from the worst of it. But in 2019 alone there were still 299 million cases around the world, according to the WHO. It also killed about 409,000 people that year. About 94 percent of those deaths occurred in sub-Saharan Africa, where the disease still runs rampant. Over half of those deaths occured in children under five years old.
Believe it or not, those dismal statistics are actually an improvement. In 2000, over 700,000 people died from malaria. Tools like insecticide-laced nets (which reduce deaths from malaria in children under five by about 20 percent) and antimalarial drugs have brought that number down to around 400,000 deaths. But these numbers haven’t budged much since 2015.
There’s hope that endorsing a malaria vaccine now will jumpstart progress yet again.
It’s something of a marvel that Mosquirix even found success, given how challenging Malaria vaccines are to create. Malaria is caused by one of five different parasites, but the parasite responsible for most severe cases is called P. falciparum. It’s transmitted when an infected mosquito (who probably picked up the parasite from an infected person) bites someone else, releasing the parasite into the bloodstream.
A parasite is “tremendously more complex” than a virus or bacteria—the types of pathogens vaccines usually target, Patrick Kachur, a professor of population and family health at Columbia University Medical Center, told The Daily Beast. He also serves on the World Health Organization’s Malaria Policy Advisory Group.
P. falciparum has evolved alongside humans for basically our entire existence, so its genes are no strangers to adapting new ways to slip through the cracks of the human immune system. Grimberg noted that malaria parasites can enter a red blood cell in 22 different ways.
There are other barriers facing malaria vaccines that have more to do with society than science. There are only about 2,000 cases of malaria in the US each year, for example. It’s a relatively low-priority for rich countries. Kachur, who also serves on the WHO’s Malaria Policy Advisory Group, said it’s a constant challenge to get pharmaceutical groups to invest in vaccine development for malaria-endemic countries, which are typically much poorer. Conducting scientific studies in African communities, where health resources are scarce, only exacerbates the reticence.
Mosquirix, manufactured by drugmaker GlaxoSmithKline, is the first malaria vaccine to overcome that laundry list of obstacles.
The vaccine consists of two major pieces: the first is a protein usually secreted by the P. falciparum when it’s in an early stage. The second piece is an adjuvant—a chemical booster that revs up the immune system.
Over the course of a four-shot regimen, the supercharged immune system learns to recognize the parasite’s calling card. It’s designed to intercept parasites during a key phase: when they’re still floating around in the bloodstream, but have yet to take refuge in the liver. This phase, said Grimberg, literally lasts minutes.
A Phase III trial on over 15,000 children and infants conducted over four years reports that the three main doses of the vaccine plus one booster was about 45 percent effective against severe malaria after one year. But that efficacy plunged to about 36 percent over the course of four years. Another smaller trial on 500 children showed a more dramatic decline. Vaccine efficacy began around 56 percent after year one, but was close to zero after four years.
This most recent approval comes in the midst of an ongoing pilot study in Ghana, Kenya, and Malawi that has delivered vaccines to more than 800,000 children. It’s reduced severe and deadly malaria cases by 30 percent, according to the WHO.
In a world that’s currently quibbling over COVID-19 vaccines with far higher efficacy, that fifty percent figure may feel low. It is low, said Grimberg. And more critically, Mosquirix hasn’t been definitively proven to prevent deaths. But there is evidence it may do so anyway, by combating severe disease. One 2020 study used mathematical modeling to estimate that, if it was distributed to countries with lots of malaria cases, it would prevent 23,000 deaths in children under five each year.
“Having seen many kids pass away from malaria, you try anything you can think of to save these kids, and I think that's what [WHO] is looking at,” said Grimberg.

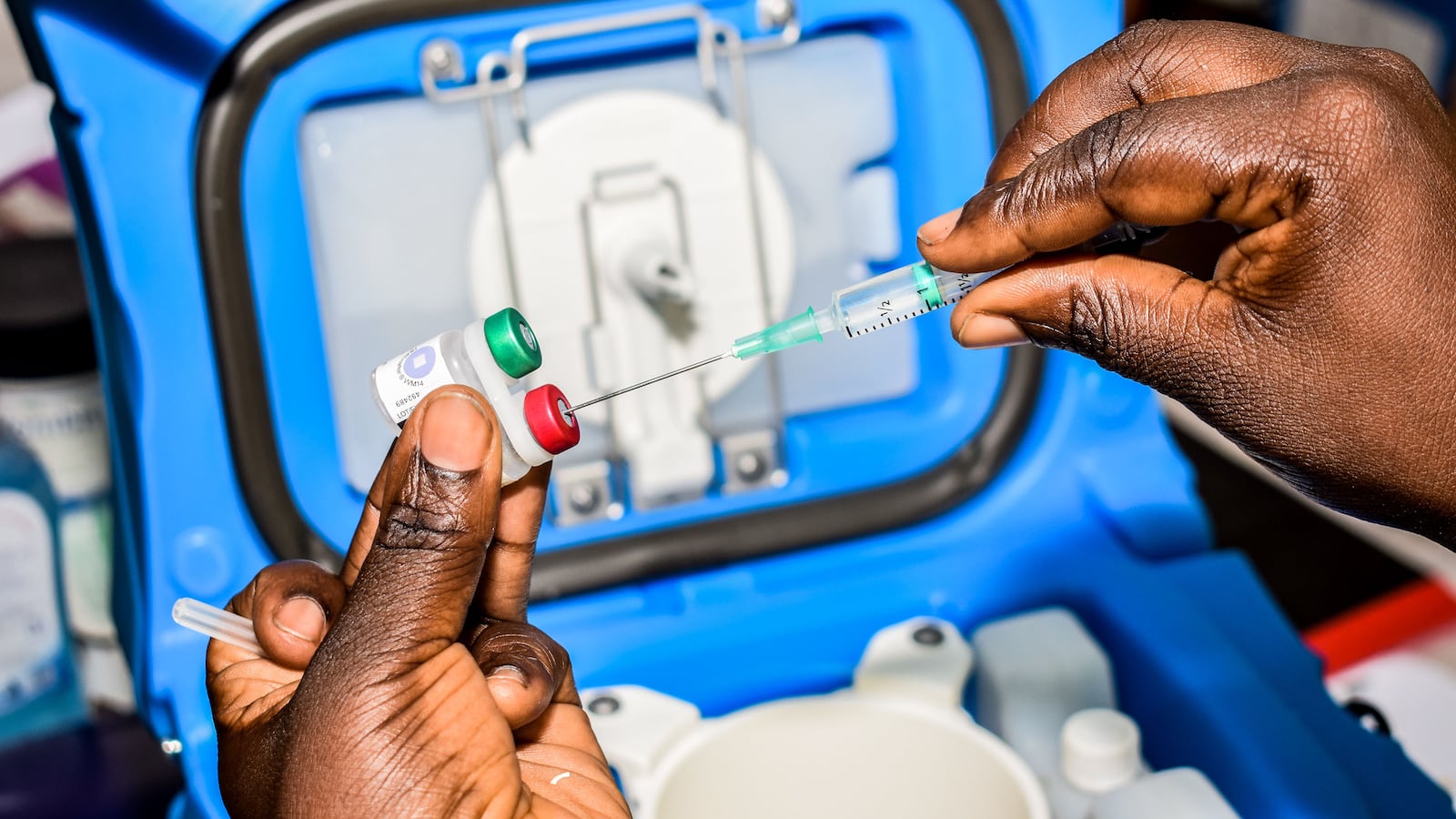
A child gets the malaria vaccination at Yala Sub-County hospital, in Yala, Kenya. Most deaths from malaria in sub-Saharan Africa occur in children under 5.
Brian Ongoro / AFP via Getty ImagesIt might also be appropriate to think of this vaccine not as a replacement for drugs or insecticide-laced nets, but as a supplement to them. “That additional efficacy on top of mosquito nets and on top of good diagnosis and treatment when people do get it, could save tens of thousands or even hundreds of thousands of lives,” said Kachur.
Another silver lining, noted Kachur, is that although some vaccine hesitancy may emerge, it hasn’t proven to be a huge issue in this trial—suggesting Mosquirix is a vaccine people will actually get.
“Some media reports and organized groups expressed hesitancy about it,” he said. “None of the countries reported seeing a difficult time recruiting patients to come and get this vaccine alongside their other childhood immunizations.”
The next step in getting it out into the world comes down to convincing the Global Alliance for Vaccines and Immunizations, called GAVI, to help countries buy it in bulk.
There’s still a long way to go when it comes to developing (and distributing) a malaria vaccine. On one hand, Grimberg thinks an mRNA vaccine, like those used to combat Covid-19, might do a better job in the long run. “I think that's probably where we're going with this technology,” he said.
But that could be decades away. This vaccine already exists—and it could probably help save thousands of lives.