It was a normal Sunday night for my patient. He mowed the lawn, cleaned the garage, and was ready for a night of watching football with his friends. David Smith was recovering from his latest round of chemotherapy for a malignant brain tumor, but for the most part, he was feeling energized. Diagnosed almost four years prior, David had outlived most of the people he met with the same diagnosis—a malignant brain tumor, Glioblastoma Multiforme—and he was proud of it, and I was proud of him.
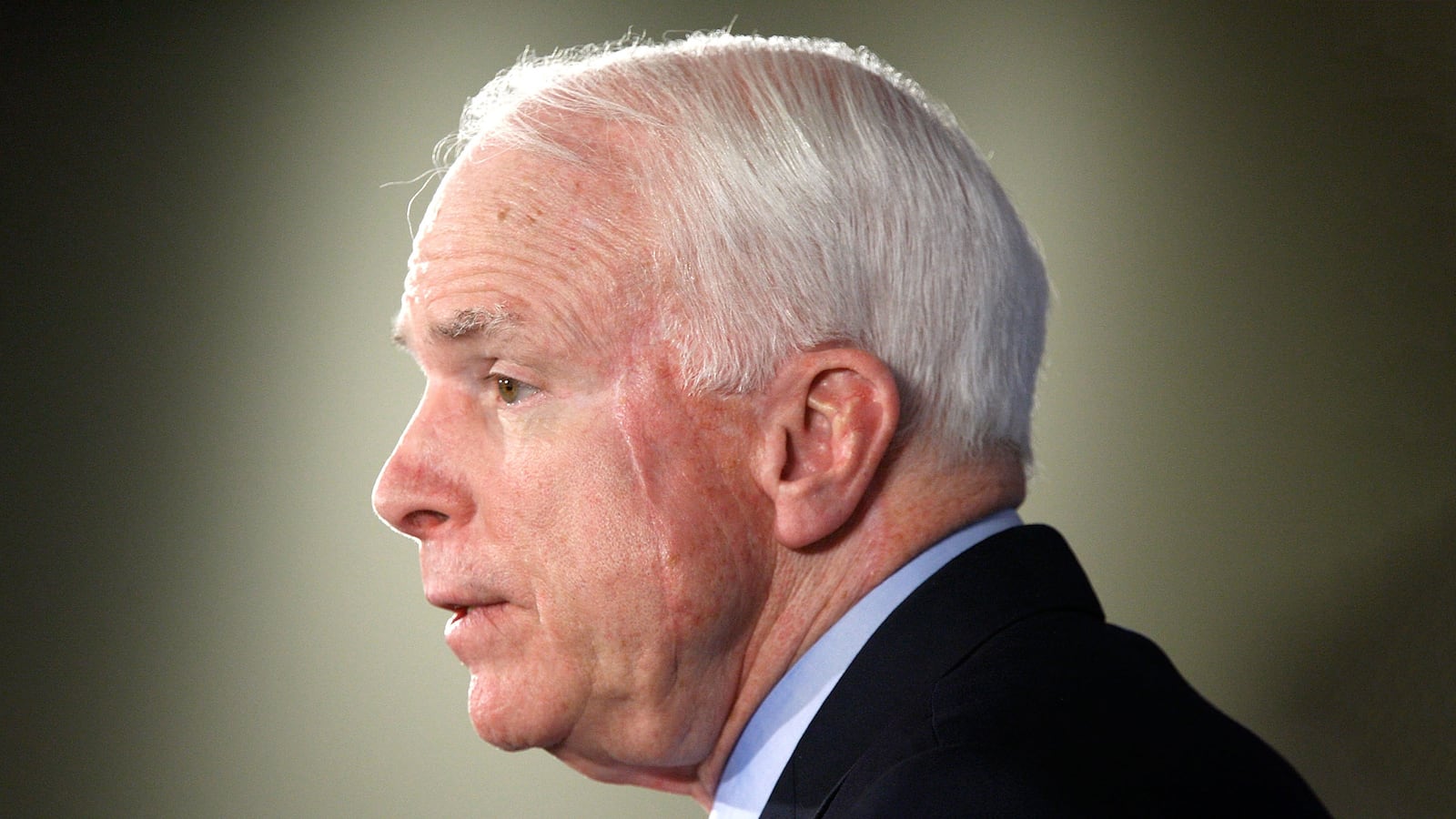
These stories are few and far between, when you care for a GBM patient, you know their days are ultimately numbered but they can outlive the very worst of the prognoses. Senator McCain is a patriot, who fought for our country, and served his people—his diagnosis is real, and the challenges are great. I am all too familiar with the road he must travel, but as he has done in the past—he will face his obstacles with great valor.
I feel for him and his family. Though in the last 20 years we have made great strides in understanding the molecular genetics of GBM, we have only extended life expectancy by a matter of months. Without treatment, GBM can be terminal in as short as 3 months. The 2-year survival rate is approximately 17 percent for patients between 40 and 65 years old.
David had done exceptionally well, but that night as he was enjoying the football, he needed to use the restroom. All was well, until he tried to stand up for the commode. He couldn’t do it, his brain was telling him to get up but his legs wouldn’t move. He knew something was wrong, he couldn’t feel his legs and he couldn’t move them. Could this be a stroke? Or how about a seizure? David had initially had seizures which is what led to his diagnosis in the first place.
Fast forward to the emergency department, and after an MRI of his brain and spine—David had an extremely rare diagnosis. A new tumor, compressing his spinal cord—disabling his legs. All of his muscles from the waist down were weaker by the minute and his sensation to his feet were disappearing. We placed a catheter in his bladder and returned over 1L of urine.
We rushed to the operating room to see what could be done to help. As I opened the spinal canal, and then the dura, my heart sank. One look at his sick spinal cord and I knew it would be very hard for me to face David’s family. David had a new diagnosis, one even more rare – metastatic GBM to the spinal cord. There wasn’t much I could do other than provide more room for his spinal cord and obtain a diagnostic biopsy sample, his treatment regimen would be radiation and chemotherapy.
The underlying cause of GBM is unknown but is thought to be a disease that arises from astrocytes, the support cells of the brain, and is typically found in the cerebral hemispheres. Most cases of GBM arise directly from mutations in healthy cells. However, a small number may transform into GBM from a previously existing lower grade tumor.
While surgery and radiation therapy play a large role in the treatment of GBM, many scientists are focusing on the role of the immune system. Immunotherapy has emerged as a promising strategy for combatting cancers like melanoma and lung cancer. For decades, prevailing wisdom suggested that the brain was “immune-privileged,” meaning that the immune system had limited access and efficacy there. However, this dogma has been challenged and immunotherapy for GBM has become a burgeoning field of research. The main classes of GBM immunotherapy are checkpoint blockade therapy, cancer vaccines, oncolytic virus therapy, adoptive T-cell therapy, cytokine therapies, and macrophage activation.
Checkpoint inhibitors
The key job of the immune system is to be able to tell “self” (your own healthy body’s cells) from “non-self” (cells that are abnormal, like cancer cells). One way which the immune system accomplishes this is via “checkpoints,” or on/off switches, that can trigger (or inactivate) the immune response. Cancer cells can sometimes use these signals to trick the immune system into leaving them alone. Drugs which target these immune on/off switches are checkpoint inhibitors and the most well understood checkpoints involve programmed death 1 (PD-1)/programmed death ligand (PD-L1) and cytotoxic T-lymphocyte-associated protein-4 (CTLA-4). Checkpoint inhibitors have demonstrated significant benefit for melanoma and lung cancer patients, as well as in mouse models of GBM. Human studies of checkpoint inhibitors for GBM have had more modest effects than in other cancers, but there do appear to be some GBM patients who may be more likely to benefit from checkpoint inhibitors than other patients.
GBM vaccines
GBM vaccines work on the same basic principle as other vaccinations—by immunizing a GBM patient with a GBM-specific molecule, termed an antigen, in order to stimulate the patient’s immune system to target that molecule. If the immune system mounts a robust response to the antigen, the immune system may be able to specifically target tumor cells. In GBM vaccine research, many different molecules have been tested as candidate antigens, with some approaches utilizing patient-specific antigens (“autologous vaccines”) and companion molecules to jump start the immune system. However, these heterogeneous approaches require further investigation and study before they can be translated into patient-care.
CAR-T therapy
Advances in bioengineering have enabled more directed manipulation of cells. Engineering of T-cells, a critical contributor to the immune response, has allowed researchers to generate tumor-seeking cells. Specifically, chimeric antigen receptors (CARs) are molecules on the surface of T-cells that can be engineered to target specific cancer antigens. The process involves taking a blood sample from a patient and extracting the T-cells, genetically modifying the T-cell to have CARs, and then re-introducing these modified T-cells into the patient. The CAR T-cells then go on to target the patient’s cancer—these CAR T therapies have generated significant and durable results for patients with certain leukemias and lymphomas. In December 2016, a report published in the New England Journal of Medicine, described the successful treatment of a GBM patient with CAR T-cells and just this week, a study of 10 patients with recurrent (relapsed) GBM further demonstrated the possibility of CAR T-based therapy for GBM.
Now more than ever do we need to invest in science, technology, and health care. The well being of our future nation greatly depends on the decisions we make today. Funding for science is quickly evaporating, but we continue to push on, fighting for the next potential break through.
Senator McCain is an American Hero, and dedicated civil servant. He has worked hard to represent his party and the people of his state, and I know he and his family understand the challenge that lies ahead. I am hopeful that immune modulation will prove to patient extended survival, only time will tell how close we are to helping GBM patients.