If we could artificially grow a real, working organ with the complexity of a lung or heart outside of the lab and customize it to match someone’s very own tissues, we could completely turn around the organ transplant crisis that kills 17 people in the U.S. each day.
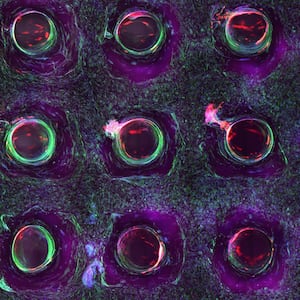
One breakthrough that has inched us closer to this reality is the creation of miniature organs, called organoids, that resemble the brain, kidney, lungs, stomach, liver, and complex tissues. These organoids aren’t just a hopeful, futuristic solution to organ shortages or transplant rejection—scientists are using them to understand how humans and diseases develop.
But a challenge to this undertaking is seeing what exactly is going on inside the organoid—how its cells are behaving and interacting with each other, how they respond to new stimuli like drugs or growth hormones—without being invasive or damaging.
ADVERTISEMENT
In a study published this week in the journal Biosensors and Bioelectrics, researchers at Washington University in St. Louis and Michigan State University in East Lansing grew living heart organoids that can beat and contract just like normal human hearts can. They tracked the growth of a heart organoid using a novel imaging device called optical coherence tomography (OCT)—which could offer scientists a three-dimensional, behind-the-scenes view of an organoid as it grows and responds to its environment, and perhaps help lead to new insights that could push forward the pursuit of artificial organ development.
“You can think of OCT as an optical analogy to ultrasound,” Chao Zhou, a biomedical engineer at WUSTL and co-author of the study, told the Daily Beast. In an ultrasound, a probe sends out a beam of sound waves into the body. Whichever sound waves reflect back, create the image you see on the screen. Similarly with OCT, Zhou said, near-infrared light waves project onto the growing organoid, and a nearby detector collects the reflected waves and draws an image from them.
Because near-infrared light waves are much shorter than sound waves, the technique allowed the researchers to see the smallest, itty-bitty details of an organoid down to the one-thousandth of a millimeter.
Zhou and his colleagues were able to watch a heart organoid grow from a small clump of stem cells to a larger blob that formed connecting chambers and valves, and even spontaneously contracted like a real heart within days.
There are still a few minor design kinks to iron out in order to make OCT a valuable tool to scientists working in tissue engineering. Because the OCT device is outside of the incubator where growing organoids are kept, the researchers had to move them back and forth between the OCT device and the incubator.
“When we image the organoids outside the incubator, they’re not in their native environment and a lot of function may change when you change the environment,” Zhou said. In the future, the team hopes to create a sort of two-in-one contraption integrating OCT into an incubator. This would cut out the manual work and dial up how frequently scientists can monitor an organoid, whether hourly or minute-by-minute versus a span of days.
OCT is already being used to study cancer using tumor organoids, Zhou said. But improving the monitoring frequency would be useful in studying a drug’s effects on an organoid, allowing scientists to immediately see in real-time how cancer drug candidates or substances like alcohol affect tissues. Getting real-time information would even help track down the moment an abnormality pops up during embryonic or organ development.
And when it comes to creating organs for transplantation, Zhou and Ming are hopeful OCT can help scientists overcome the technological limitations impeding a wider understanding of all the factors shaping the function and three-dimensional structure of organs like the heart.
“For example, we don’t really understand how the human heart forms from embryo to adult,” Yixuan Ming, the study’s lead author, told The Daily Beast. He added that the heart organoid the researchers created from stem cells resembled more so a fetal heart rather than an adult human heart.
It will be a long time until we will see organoids reaching a potential that can address diseases, persisting organ shortages, or help transplant patients grow their own organs. But OCT might improve our understanding of the human body well enough that the time to get there shrinks by a great deal.