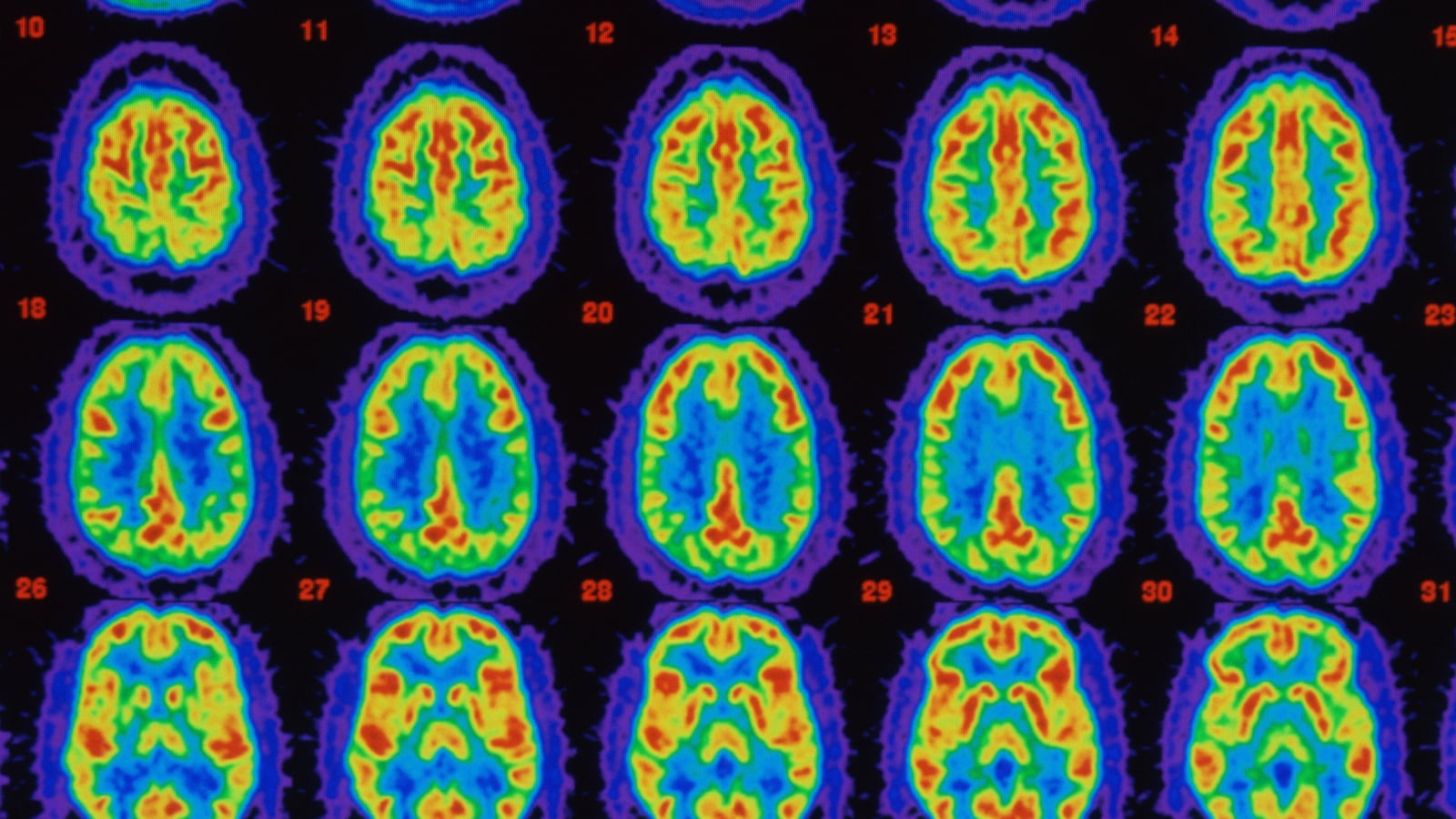
A drug in early animal trials has shown promising results, appearing to reverse the symptoms of Alzheimer’s disease in mice.

Additionally, in mice, the treatment reduced inflammation in parts of the brain that are associated with memory and learning, according to a study led by Susan Farr of Saint Louis University School of Medicine, published in the Journal of Alzheimer’s Disease.
The mice were engineered to produce a mutant form of human beta amyloid, one of the proteins associated with Alzheimer’s disease. In a previous study, the researchers had tested mice that naturally overproduced mouse beta amyloid; this step was to see if the drug would work with the human version. Both types of mice showed impaired learning as they aged, much like humans with Alzheimer’s disease.
Two groups of mice were tested: the mutants, and wild-type mice. The wild-type mice were given random compounds, along with half of the mutants. The other half of the mutants received the experimental drug, called antisense oligonucleotide or OL-1. They were then tested in mazes, to see how well they learned and remembered while exploring a new location, and in recognizing objects. The genetically engineered mice that received OL-1 did about as well as the wild mice.
“It reversed learning and memory deficits and brain inflammation in mice that are genetically engineered to model Alzheimer’s disease,” Farr said in a statement released by the school. “Our current findings suggest that the compound is a potential treatment for Alzheimer’s disease.”
About 5 million Americans who are 65 or older have Alzheimer’s disease now, and that number may rise to 16 million in 2050, according to the Alzheimer’s Association, an advocacy organization for the disease. There is no cure.
Four drugs are currently used in Alzheimer’s disease: Aricept, Exelon, Reminyl, and Namenda. They all temporarily treat symptoms of memory loss, but lose effectiveness as the disease progresses.
Unlike these drugs, OL-1 doesn’t target symptoms. Its molecules bind to messenger RNA, allowing certain genes to be “turned off.” Here, the blockage of RNA prevents extra amyloid from being produced by targeting its precursor protein and making less of it. The hope is that by lowering the amount of amyloid, fewer mind-robbing plaques would appear—either slowing the disease’s progression or halting it entirely.
OL-1 hasn’t been through the toxicity trials needed to determine if it’s safe for human use. Many promising treatments for diseases don’t make it past this step into Phase 1 testing in humans. And even that’s just the beginning. Only about 10 percent of drugs tested in Phase 1 go on to make through the FDA, according to a January article in Nature Biotechnology.
In fact, more than 100 drugs for Alzheimer’s disease have either failed in development or been abandoned. Beta amyloid, which OL-1 is meant to lower, was first implicated in the disease at its identification by Alois Alzheimer in 1906. Many researchers believe that the dementia from Alzheimer’s disease is caused by an accumulation of beta amyloid in the brain, forming plaques that choke healthy cells, leading to the loss of neurons and, eventually, problems with thought.
Previous drugs targeting amyloid precursor protein, or APP, have failed. Eli Lilly & Co.’s drug to inhibit one of the chemicals that slices APP into beta amyloid not only failed in a final-stage trial, it was worse for patients than a placebo. Another drug company, Myriad, tried a similar route, and also failed in clinical testing.