Immune therapies have rewritten the game when it comes to cancer treatment, earning the “fifth pillar” label next to more tried and true treatments like radiation therapy, surgery, and chemotherapy. And no immunotherapy has garnered quite the same excitement as CAR T-cell therapy, first approved in 2017 by the Food and Drug Administration to treat a form of acute lymphoblastic leukemia. At the time, then-FDA Commissioner Scott Gottlieb called the approval “a new frontier in medical innovation,” and it seemed like the possibilities for CAR T were near-endless.
Flash-forward almost six years, and six therapies have been approved for blood cancers, including lymphomas, leukemia, and multiple myeloma. There’s no question that when CAR T works, it works incredibly well. But why it doesn’t work for the majority of patients or cancer types has befuddled researchers.
“We have patients who, several years ago would have no options and because of this new therapy they are now in long-term remissions,” Jakub Svoboda, an oncologist at the University of Pennsylvania, told The Daily Beast. “But with all of that, what I see in my clinic is that the number of patients who greatly benefit from this treatment is still well under 50 percent” as a third-line treatment for a type of lymphoma, he added.
CAR T therapies also haven’t yet been expanded to treat solid tumors, which make up the majority of cancers. The immune therapy hasn’t been able to crack physical barriers, idiosyncratic tumor cells, and a suppressive microenvironment that characterize these cancers. But a new generation of CAR T therapies are emerging, equipped with highly effective small molecules that scientists hope will solve their low success rate for both blood cancers and solid tumors. Known as “armored CAR T,” these infusions have been boosted with additional layers of protection and cancer-fighting proteins. Early research shows that the armored flavor of CAR T might have what it takes for immunotherapy to go the extra mile.
“We’re making these cells and sending them on this really difficult adventure through different terrains and different problems—so we need to give them a set of tools,” Wendell Lim, a cellular and molecular pharmacology researcher at the University of California, San Francisco, told The Daily Beast.
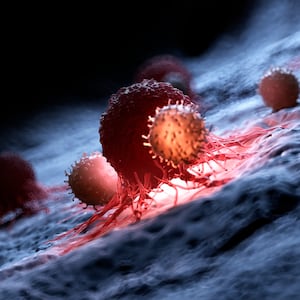
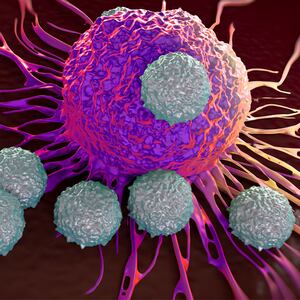
Briefly, immunotherapy can boost or restore the body’s immune system by lowering cancer cells’ defenses, priming the immune system’s T cells to destroy tumors, or—in the case of CAR T-cell therapy— genetically editing a patient’s T cells. Scientists do this by isolating a patient’s T cells from their blood and inserting a gene for a chimeric antigen receptor—a type of synthetic protein that has been specially made to bind to another protein present on the surface of that patient’s cancer cells. Then, upon infusing these modified T cells back into a patient, the immune fighters will recognize and destroy the tumor cells when the patient’s normal T cells have failed.
That, at least, is the idea. But when CAR T doesn’t work, a few factors could be at play. One, Lim said, is the tumor microenvironment, the set of chemicals and structures present in solid cancers that naturally suppress pushback from the body’s immune system. Tumor heterogeneity is also a factor—depending on the type and stage of cancer, tumor cells may not express the protein that the CAR T cells’ receptors have been designed to recognize, blocking the ability of the CAR T cells to attack the cancer Finally, there are physical barriers on the outside of a solid tumor that can even prevent the T cells from entering inside to destroy the cancer.
Armored CAR T is meant to overcome these difficulties. With this form of therapy, not only are T cells engineered to express a tumor cell’s surface protein, they are also given potent cargo often in the form of small proteins called cytokines. If deployed on their own, such molecules can be toxic—but pairing them with T cells designed to release them at the tumor site and nowhere else represents a promising new strategy.
Svodoba is helping to lead a clinical trial using armored CAR T-cell therapy to treat patients with non-Hodgkin lymphoma for whom previous CAR T therapy has failed. Last month, he presented findings that the first seven patients treated with this therapy all responded to it and were alive eight months after receiving it. Svoboda said an important additional finding was that toxicities experienced by the patients—a concern with cytokines—were comparable to those from traditional CAR T therapy.
Lim’s team is also working on an armored CAR-T therapy, with the potential for it to be used to treat solid tumors. In a paper published in Science on Dec. 16, he and his colleagues designed T cells to release a cytokine directly to the tumors of mice with pancreatic cancer and melanoma. In the study, they wrote that these cancers are “nearly completely resistant” to treatment with traditional CAR T, but releasing a cytokine allowed the engineered T cells to get past the tumor microenvironment—effectively solving one of the issues that has set the therapy back.
“The way to think about the future of CAR T-cell therapies is developing reliable tools that solve certain problems and coupling them together in one package,” Lim said. The researchers hope to begin patient trials of an armored CAR T therapy within the next two years.
Getting these treatments to the clinic won’t be a speedy process—more trials will be needed to make sure that armored CAR T can be effective while reducing toxicity as much as possible. Personalized immunotherapy can also take time to produce—time that cancer patients may not always have—and are often expensive. Still, Svodoba said that efforts are underway to make therapies more accessible, and that the cost may be worth it if armored CAR T can be effective in the long run.
“If one infusion of an expensive product can result in long-term remission or a cure, investing in that type of product makes a lot of sense to me.”