Alzheimer’s disease has no cure—yet.
It was discovered in 1906 by its namesake, Dr. Alois Alzheimer. But it wasn’t until the 1980s that research on causes and prevention began, so it’s only been studied for the past 40 years, making the research field comparably young compared to other conditions like heart disease and cancers.
But two researchers are turning what we thought we knew about Alzheimer’s on its head.
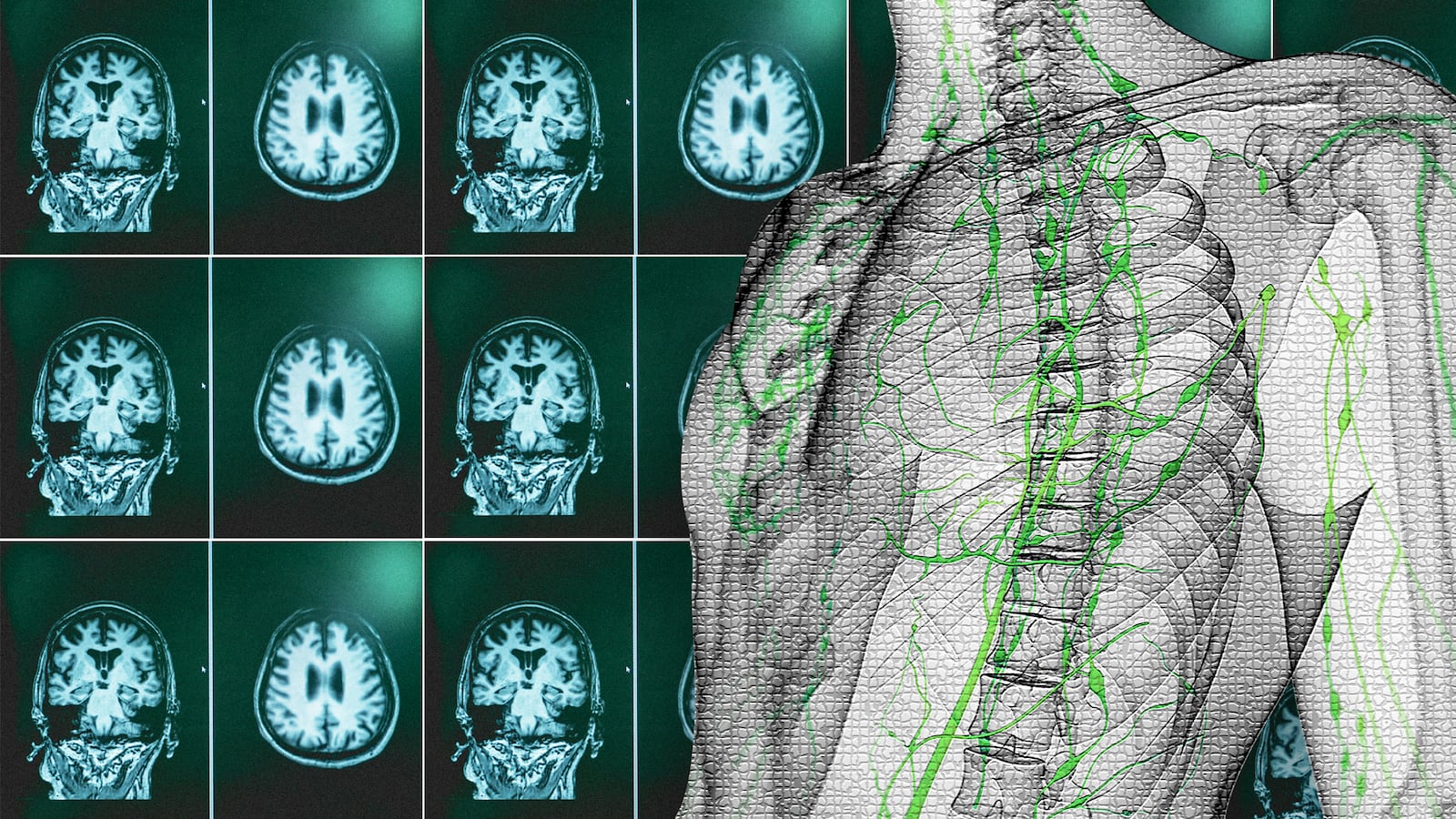
Here’s how: Beta-amyloid, a sticky protein that clumps together and kills brain cells leading to cognitive decline, has been heralded as what we need to understand to cure the disease, according to Alzheimer’s Association. Researchers have been studying ways to find genetic mutations linked with beta-amyloid production or drugs to target the protein before it causes too much damage.
But Rudolph Tanzi and Robert Moir, two Harvard researchers focusing on Alzheimer’s, are looking at the protein in a different way.
Since 2010, Tanzi and Moir, have shown that amyloid-beta, a protein linked to Alzheimer’s, is actually antimicrobial, meaning it’s developing in the brain by fighting against something.
“We assumed that amyloid-beta protein in the plaque is just an abnormality that happens with age, but over the last 10 years, Rob and I discovered that the amyloid-beta protein actually plays a role in the brain by protecting the brain against infection,” Tanzi said.
This just so happens to connect with the body’s ancient immune system.
“Turns out, our most ancient immune system, before we had adaptive immunity, had little baby proteins, antimicrobial peptides, and when they saw bacteria or a virus or a fungus, they would stick to it and clump it up into a ball and the peptide would grow into a spiral like spaghetti and trap it like a fly trapping a seed, and that is one of the most classic ways that our primitive innate immune system protects us,” he said.
One of these known peptides is called LL-37, which Moir and Tanzi discovered was molecularly similar to the amyloid-beta protein. Moir and Tanzi started with a petri dish, putting Alzheimer’s genes in it and adding a microbe to the dish. Amyloid-beta plaques built up overnight.
“This changes the paradigm,” Tanzi said. “People thought these plaques formed over decades.”
Along with the new hypothesis came the questions, though: Was amyloid-beta forming in the brain to protect it from something? If so, what exactly? Is there a way to ward off what it’s protecting the brain from? And, of course, is this too crazy to be true?
“I was totally gobsmacked when I first heard this story. I was very skeptical,” Sam Gandy, an Alzheimer’s professor and researcher with Mount Sinai, told The Daily Beast. But research Gandy has since seen out of Mount Sinai and Banner Alzheimer's Center in Phoenix made him think Tanzi and Moir might be onto something. There are also other amyloids in the body—in semen, that can help block HIV—that strengthen Tanzi and Moir’s model regarding the likelihood that something similar happens in the brain, Gandy said.
David M. Holtzman, MD, a neurology professor at Washington University School of Medicine in St. Louis who researches genetic risk factors for Alzheimer’s but hadn’t worked with Tanzi and Moir, was skeptical as well.
“I was mostly surprised, I never thought about it as a possibility. It wasn’t that I thought this was so far out, I just thought, ‘This is new, this is very different,’” he told The Daily Beast.
The next step is to figure out how to stop the amyloid-beta before it starts, as researchers have found that treating amyloid once it’s already formed doesn’t work or halt cognitive decline.
“When you treat someone with symptoms already, it’s like trying to put out a forest fire by blowing out the match,” Tanzi said. “It’s like cholesterol: You don’t want to wait until you have a heart attack to start taking a statin.”
Tanzi said that the aim is not to wipe out the amyloid-beta completely but just to dial it down because, after all, it is protecting the brain—at least at first.
“But we do fully support that you want to prevent or stop it in its very first stages, 10 years before symptoms, you hit the amyloid,” he said.
However, Tanzi said what would truly be ideal is to not have to touch the amyloid at all but to hit the microbes that trigger the amyloid. He and Moir, with backing from Cure Alzheimer’s Fund and Open Philanthropy, are mapping everything residing in the Alzheimer’s brain by looking at autopsies in Alzheimer’s patients and those who are just as old but didn’t have the disease.
Tanzi said it could lead to a test for young adults that would see if their brains are susceptible to the antibodies that cause the plaques. This would be true preventative treatment, an idea that’s long-been thought to be impossible in the Alzheimer’s world.
“The whole mindset is changing around Alzheimer’s to treat at the stage of pathology and not wait for the symptoms to occur,” Tanzi said. “You have to treat people before they have symptoms, like you treat HIV before it turns into AIDS and like cancer, you don’t wait until you have symptoms of cancer, you treat the tumor.”
Tanzi admits it’s unclear if this kind of preventative treatment will even work and, if it does, it’d be a long way out from clinical application. But still, in the face of a disease that’s been incredibly difficult to treat for 100 years, there’s hope. And this time, a new, different kind of hope.