When Conor McGinn, head of the Innovation and Robotics Lab at Trinity College Dublin, and his team began piloting their robot Stevie in the U.S., they were surprised to find that many of the applications we might anticipate robots doing, such as fetching objects, aren’t what people actually want.
“People want quality of life improvements. They want to have more fun, more social interaction,” McGinn said.
Because of that observation, Stevie’s priority shifted would be to combat isolation and loneliness by bringing people together through activities such as game-playing.
And they found a surprising audience starving for attention and friendship: the elderly.
And there’s quite a market for Stevie. Elderly populations around the world are soaring, doubling to an estimated 2.1 billion people worldwide over the age of 60 by 2050. But the workforce caring for the elderly is dwindling. Robot nurses such as Pearl and RIBA already help mitigate staffing shortages in countries such as Japan, which has the highest proportion of elderly people of any country, and whose government directs considerable funds into the development of care robots.
Now, nursing homes and assisted living facilities everywhere are beginning to recognize the benefits of robotic caretakers.
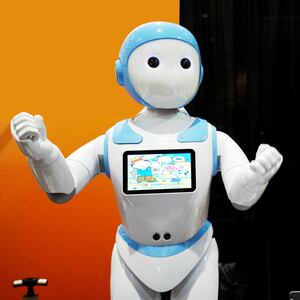
Sayabot, a humanoid service robot created by Asimov Robotics, is one of these robots. A mobile robot with dexterous arms, a humanoid face with eyes equipped with cameras, and speech capabilities, Sayabot can be customized for patient use and is already seen in banks and restaurants.
According to Jayakrishnan T., CEO of Asimov Robotics, the robot assisted patients between 60 and 85 years old in clinical trials last year, performing tasks such as helping patients use the restroom, providing mental stimulation through conversation and games, 24/7 monitoring, and dispensing food, drinks, and medicine. Sayabot and other “care-bots” can also call for human assistance if there’s an emergency.
But creating a robot that interacts productively with patients is more challenging than designing a robot for other customer service interactions—the stakes are higher, as is the need for sensitivity.
For one thing, the appearance of a care-bot is important—it should be human-like but not so much that it triggers an “uncanny valley” response.
“Sayabot’s design is based on studies that have found a ‘sweet spot’ between human and machine,” Jayakrishnan told The Daily Beast.
Details matter, such as Sayabot’s eyelashes, which humanize its face enough to make it appear engaged, but not creepy. Jayakrishnan’s team has also developed Sayabot’s voice, volume, and modulations to be “pleasant”; a robot can’t be helpful if its voice is grating or frightening.
Sayabot also monitors patients’ gestures and facial expressions to determine the best strategy and demeanor for care. “Even if the robot has to nag a patient by repeatedly reminding them to take their medicine, it will be thoughtfully done at the best suitable time,” Jayakrishnan said. That’s based on data gleaned from clinical trials, as well as from individual patients; over time, these robots learn what approaches work best for the people with whom they interact.
So how do humans respond to Sayabot? In experiments with Sayabot, some patients expressed apprehension and skepticism about having a machine around instead of a human for care. But according to Jayakrishnan, it only took about two days for patients to grow comfortable with the robot.
While situations for which robots have not been expressly trained pose challenges and require constant feedback and updating, every new situation helps robots like Sayabot and their designers learn more about the functionality necessary to provide effective care. And unlike humans, robots don’t get tired or short-tempered, which helps ease patients’ stress and worries about being burdensome.
Being freed from the worry that they’re inconveniencing or irritating human caregivers helps facilitates a real relationship between patients and the robots looking after them, and it’s not surprising that humans soften towards their care-bots. When a French hospital brought in Zora, a friendly-looking robot just under two feet tall with sensors and speech capabilities, residents developed attachments to it. The same goes for PARO, a robotic seal that elicits emotions and boosts interactivity among users. Zora and PARO don’t fulfill medical tasks and aren’t caretakers in the traditional sense, but they help mitigate the loneliness that plagues residents of assisted living and nursing homes.
Being friendly and fun might not seem like health care, but given how loneliness and isolation adversely affect people’s health and motivation to live, it makes sense to couple companionship and care.
Which brings us back to Stevie. One of the most interesting results of the trial programs with Stevie is how much residents enjoyed being part of the focus group. They got to provide feedback about what they liked and didn’t like, and what they want and didn’t want, which facilitates feelings of ownership and purpose.
“The residents wanted to help create the robot. They wanted the responsibility and took pride in helping to shape Stevie,” McGinn said.
Soliciting and implementing feedback from residents has been so integral to Stevie’s benefits that McGinn realized that process shouldn’t end when the pilot programs do, but should be part of the product offering.
“Residents organize committees to show each other how to use the robot. They’re facilitators, not just customers. Stevie gives them motivation to do things that are good for them,” he said. The unanticipated benefits of using Stevie outweigh the expected ones, which suggests that more paradigm shifts might arise from the use of such robots in facilities.
The biggest concern about robotic caregivers is that they shift care away from humans and become an excuse to pass off the care of the sick or elderly onto machines. “It’s potentially very dangerous taking people out of the loop,” McGinn acknowledged, “but I don’t think that’ll happen anytime soon. The tech isn’t even close to being able to circumvent all people.”
Pilot programs with Stevie were illuminating, especially regarding assumptions most of us make about what drives caretaking needs.
“People who are worried about tech replacing people haven’t spent time in nursing homes. The people who work with these patients don’t spend quality time with patients—they’re stressed and getting beeped constantly. The truth is that older people are alone all the time, starved of care and interaction,” McGinn said, emphasizing that robotic caregivers don’t replace interactions—they add to them, especially in situations where those interactions aren’t currently taking place.
While robots such as Stevie might not be affordable for individuals, they’re cost-effective solutions for facilities in which a single robot could assist 20 people.
According to Kimberly Stanley, Healthcare Sector Leader with EYP, an architectural design firm that works with healthcare organizations, it’s easier to “picture robots assistant with more time-consuming jobs that are not patient-facing. However, it doesn’t take much imagination to envision a day when empathetic, patient-facing robots are commonplace.”