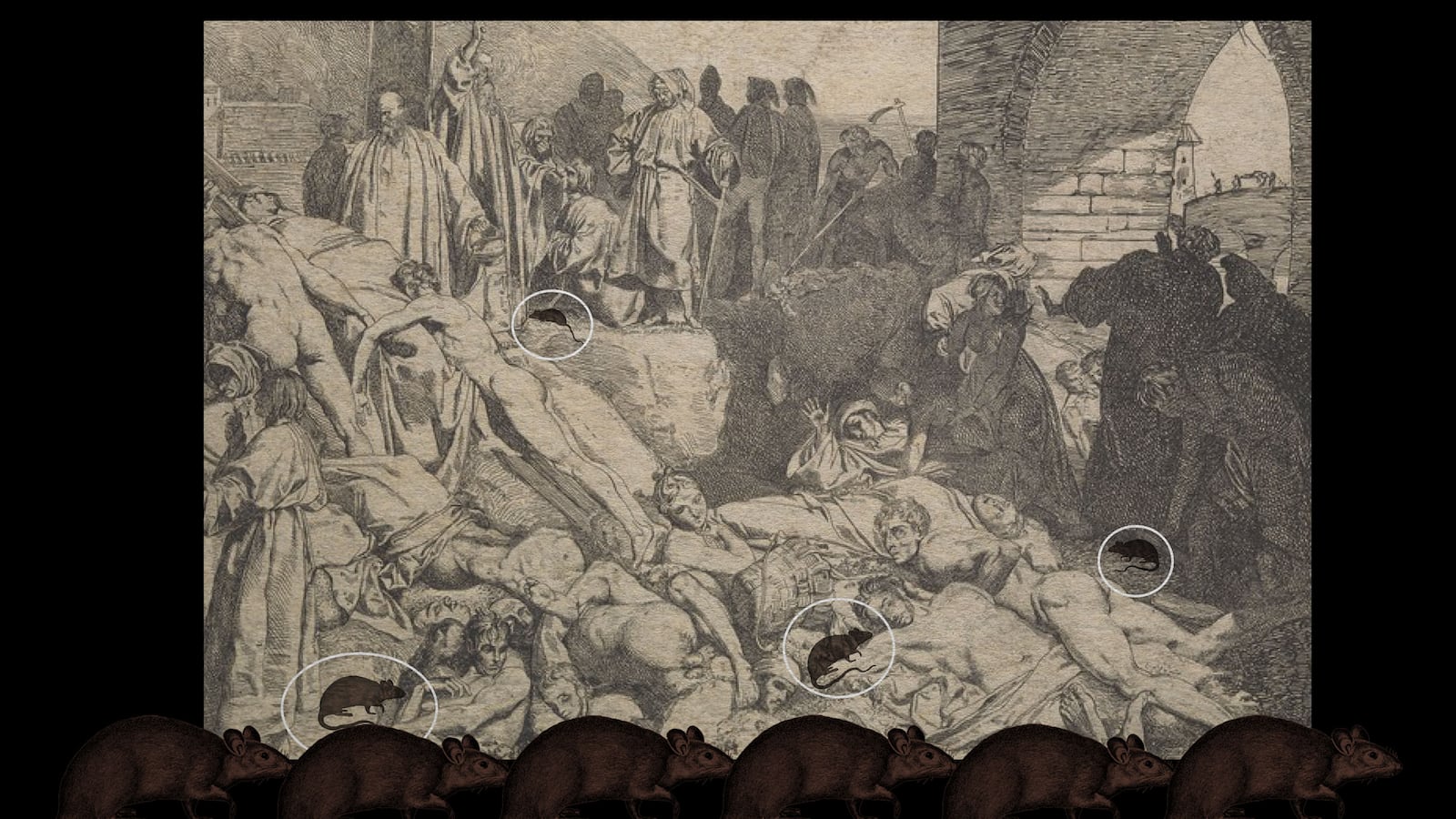
There is a legend that you may have heard about the arrival of the Black Death in Europe. According to a story told by Italian notary Gabriele De’ Mussi, plague arrived in 1346, when “Tartars” attacking the city of Caffa in the Crimea came down with a mysterious illness. The dying Mongols decide to catapult the bodies of their dead over the walls of the city to infect the inhabitants within. That illness was bubonic plague. From there, the story goes, the plague spread throughout Europe, killing between 30 percent and 50 percent of the population.

Bubonic plague victims in a mass grave in Martigues, France.
S. Tzortzis/CDC/Wikimedia CommonsWhile the impact of the Black Death in the 14th century is undeniable, this does not mean that the narrative about how or when it began is accurate. New research that fuses paleogenetics, historical detective work, ecological studies, and biology is challenging what scientists and historians thought they knew about the plague with some important consequences. As it turns out, the plague that ravaged Europe in the 14th century began much earlier than thought. The culprit wasn’t Mongols’ biological weapons (there’s no other evidence that they weaponized corpses), it was something much smaller… and cuter.
While scholars have been interested in plagues for a while and interest in historical pandemics heated up as we encountered coronavirus, there are only a few people who can deftly navigate both the historical and scientific material. At the forefront of this interdisciplinary effort is Dr. Monica Green, an award-winning medieval historian whose work interrogates narratives about plague. She gathers up all the available forms of evidence and insists that whatever narratives we tell have to be anthropologically, biologically, and historically plausible.
One problem with writing histories of pandemics is the nature of the available evidence. Eyewitness accounts provide vivid details about symptoms and the local impact of a contagious disease, but they can only give us the roughest sense of how it spread. Then there are human remains, which are tricky. If someone died violently 2,000 years ago, archaeologists can tell that from visually examining their remains. Infectious diseases, on the other hand, rarely leave evidence in our bones so it’s difficult to determine cause of death from looking at a skeleton (the exceptions to this rule include tuberculosis and leprosy). Plague kills someone in two to 10 days, without leaving a mark. To add to our problems, most victims of contagious diseases were buried in mass graves, many of which have not been identified. With the exception of a headstone from Kara-Djigach in Kyrgyzstan we don’t have graves that can help us identify the deceased.
What we do have, thanks to paleogenetics, is molecular evidence of Y. pestis, the pathogen that causes plague, from the remains of individual human victims. The plague of Justinian, the Black Death, and the 500 years of plague outbreaks that followed the Black Death, were all caused by variants of the same bacterium. New developments in molecular biology allow scientists to gather up fragments of microbial forms and reassemble them, even from those who died hundreds of years ago. Green told me, “By retrieving whole genomes of the pathogen, paleogenetics can make possible comparisons between the strains involved in historical outbreaks and samples of the bacterium found anywhere in the world.” Comparisons of these genomes can be used “to construct phylogenetic trees (family trees) that then ‘plot’ the organism’s evolutionary development across space and time.” As it turns out, there are several branches of the bacterium Y. pestis (four primary variants, the original strain 0, and a variant from the Neolithic period). Because every genetic sample has a known provenance the geographical information is usually solid even if its dating is not. “This,” said Green, “is what allows epidemiological inferences about the direction of spread.” In other words, it allows us to track the disease.
The primary reason that we date the Black Death to the 14th century is because our historical sources told us to. When Green came to work on this subject, she wondered how science might change the picture. She took genetic estimates and realized that the data points us to a century earlier. Moreover, they were leading her east. As she followed the genetic trail, she discovered that all four of the new Y. pestis strains that came out of a “Big Bang” centered on the Tian Shan mountains in Central Asia. At that point, she told me, she asked herself “Is there something we have been missing?” In answering the question, she struck upon a furry culprit: the marmot.
As we all remember learning in school, the Black Death was “caused” by rats. In truth it wasn’t the rats but the fleas they carried that spread the disease. Nevertheless, rats, the villain of our modern histories, may have taken the fall for another rodent. Green knew that marmots were hosts to plague because field ecologists had collected evidence for strains of Y. pestis in marmots of the Tian Shan mountains. But the details of the plague’s spread were still unclear to her. At the time Green had been in dialogue with her colleague, Nahyan Fancy, a historian of medieval Islamic medicine. Fancy had been reading discussions of plague symptomatology in medical texts that pre-dated the Black Death. Green had noticed references to plague in 1257 along the path the Mongol leader Hulagu Khan took into Iraq/Iran. These examples were almost a century older than the siege of Caffa. Clearly plague was circulating earlier than others had realized. (Green and Fancy co-published an open access piece on this)
What neither of them could explain, however, was the transmission of the disease. How did Y. pestis spread from marmots in the mountains of Central Asia to the military warpath hundreds of miles away without anyone noticing it? Plague isn’t a forgotten notebook in a backpack, it needs mammals to spread. So, surely, if plague was spreading people should have been dying in its wake?
As she read widely in Mongol literature for her research, the answer fell into Green’s lap. She discovered a text by a Persian physician al-Shirazi that included the seemingly trivial detail that Hulagu was importing millet grown in the foothills of the Tian Shan mountains. At that moment, Green told me, “The skies parted and everything was clear. Some spillover event(s) had knocked plague out of its long-term hosts in marmots in the mountains of the Tian Shan. The disease moved through rodent populations at lower elevations and started spreading into commensal rodents that hung around the agricultural fields from which the Mongols obtained their grain.”
The grain fields were where contact was established with human technologies. “All you would need,” Green explained, “is a couple of mice/voles/whatever to crawl into one of those sacks of grain, bringing their bacteria-filled-fleas with them, to make a ‘plague bomb’ that could then be transported hundreds of miles in the Mongols’ supply trains.” What this means, as Green shows in an important article published in American Historical Review, is that the Black Death ‘started’ 100 years earlier than we knew. The idea that plague suddenly happens in a devastating human outbreak and subsequently evaporates into thin air is a myth. In this case it was seeded by military campaigns that took place nearly a century earlier. In fact, Green and Fancy’s findings echoed associations that Robert Hymes had already noted in 2014 between what seemed to be plague outbreaks and Mongol sieges in China.
In describing the significance of this kind of this research Professor Peter Sarris, a historian at the University of Cambridge and author of the forthcoming book Justinian—Emperor, Soldier, Saint, told me that paleogenetics “has put to rest a long-drawn out debate over the nature of the [Black Death] and whether it was bubonic plague.”
It is equally important for the identification and history of plague in different periods. Up until the historian Michael McCormick began to collaborate with genetic scientists in the early 2000s, historians couldn’t be sure what this sixth-century plague was. Once again, we relied upon our interpretation of historical sources.
Sometimes, the pathogen is found by chance. In 2019 a splashy set of articles by Lee Mordechai and Merle Eisenberg, impressed the media and academic community with the claim that the plague of Justinian had been wildly overblown. You may have read about it. According to Mordechai and Eisenberg, it the Justinian Plague was not that significant. A less well publicized accidental discovery would prove to be a sticking point. A 2018 study of the sixth-century remains of a pregnant woman from Edix Hill, a picturesque village in Cambridgeshire, England, revealed that she had died carrying bubonic plague.
Why does this matter? Well, according to the narrative supplied by Byzantine court historian Procopius, and that forms the basis for many modern histories, the plague of Justinian emerged in the middle of the sixth century and spread from Egypt up through the Mediterranean to the capital of the Empire—Constantinople. From there, historians thought, it moved across the continent to France, England, and Ireland. The Edix Hill discovery complicates this narrative.
As a brilliant piece by Sarris in Past & Present that builds on the work of others like Green and Lester Little explains, the Edix Hill strain of Y. pestis is the earliest strain of the bacterium identified in the Justinian outbreak (so far). “The probable dating of the Edix Hill burial site,” writes Sarris “suggested that the plague may have arrived in England a good century before it was attested in any written source for Britain. That the plague reached rural Cambridgeshire at the same time as it arrived in Constantinople is remarkable.” If the plague was just a blip would it have had an impression on small villages? “In other words, it appeared to be a phenomenon of potentially greater significance than even the literary sources suggested.” All major historical writers of the period mention it. It is, Sarris writes, very far from the “inconsequential pandemic” Mordechai and Eisenberg were claiming it to be.
One of the crucial takeaways from Green’s work is that “Plague is Not a Human Disease.” It may seem cruel, Green told me, to say that about a disease that killed millions of people, “but the fact remains that everything we know about plague from modern science is that it is a rodent disease, and it must persist through rodent populations if it is to survive. So maybe we were looking for the wrong thing: people were assuming plague wasn’t present if humans weren't reporting it. But what if it was moving underfoot, in a way that no humans (or very few humans) were noticing?”
Green’s work, like all studies of pandemics, has some real practical relevance for our current mid-to-post-pandemic situation. When I asked Green what she thought we should learn from her work she told me that it’s clear “that most pandemics have a zoonotic element. I can't tell you how many shivers went down my spine when I first heard that mink, and then North American deer were being infected with SARS-CoV-2.” Animals are an important vector in the spread of disease. “The plague pandemics persisted for hundreds of years in western Eurasia because they were able to create new local reservoirs. Most pandemics also have some major element of human behavior that's allowing a small outbreak to spread through major systems of human connectivity.” It’s hard to fault her logic: in 2020 a teenage boy in western Mongolia died of bubonic plague after eating an infected marmot. Plague infections continue to crop up in the western United States because of contact with local animal populations. Green herself has researched the continuing outbreaks in East Africa, where 95 percent of modern plague cases are located.
To learn from these experiences, Green said, we need to think more about “the ways human-animal-environment relations work, and how we might [ignore] the ways our disruptions of those relations can produce serious consequences.” In the case of the plague of Justinian, it seems to have been helped by environmental factors. If climate change, volcanic eruptions, and dust veils can hasten the spread of disease, we probably have to pay attention to how we treat our planet—or at least the rodents scurrying beneath our feet.